Researchers Identify Predictors of Electronic Prescribing Use in Primary Care
Although substantial investments are made in health information technology (HIT) to improve practice efficiency and patient care, widespread adoption of electronic prescribing continues to lag throughout the US and Canada, which is why one team of researchers sought to determine what variables predict the technology's successful integration in primary care settings.

Although substantial investments are made in health information technology (HIT) to improve practice efficiency and patient care, widespread adoption of electronic prescribing continues to lag throughout the US and Canada, which is why one team of researchers sought to determine what variables predict the technology’s successful integration in primary care settings.
In an attempt to identify the factors that influence implementation, Claude Sicotte, PhD, from the Institute of Public Health Research at the University of Montreal, and researchers from the Canadian Patient Safety Institute in Ottawa and McGill University in Montreal provided a free research-based electronic prescribing and drug management system to 61 primary care physicians within a single city region in Quebec who lacked any previous experience with HIT.
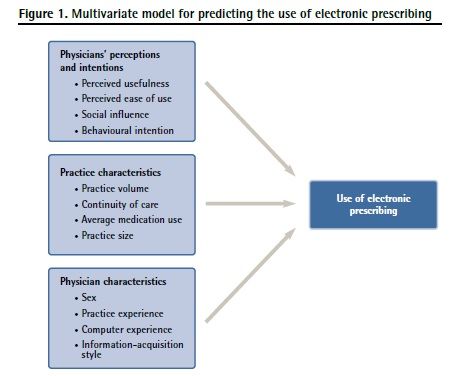
For a nine-month period between October 2005 and July 2006, the investigators tracked the physicians’ actual use of electronic prescribing and performed explanatory analyses across three variable groups of potential predictors: Physicians’ perceptions and intentions to use the system, practice characteristics, and physician characteristics. (Figure 1)
At the conclusion of their “Predicting the Use of Electronic Prescribing Among Early Adopters in Primary Care” study published in the July 2013 issue of Canadian Family Physician, the researchers found that the physicians wrote a total of 15,160 electronic prescriptions for 18,604 consenting patients; however, “physician electronic prescribing rates varied considerably, from a low of zero to a high of 75 per 100 patient visits, with a mean utilization rate of 30 per 100 patient visits,” the authors discovered.
Breaking down those statistics by physician and practice characteristics, the researchers noticed that “the highest utilization rates were for male physicians; physicians with more than 34 years of practice experience; (had) receptive and pragmatist (approaches); physicians with more than 10 hours of computer use per week; physicians with mean practice sizes of less than 1,500 patients; and physicians with patients with an average of three or more medications.” In terms of physician perceptions and intentions, the investigators established that “higher utilization rates were seen for physicians who strongly believed electronic prescribing would improve continuity of care, provide professional autonomy, be useful, be easy to use, make work easier, and be viewed positively by colleagues.”
generally predict HIT adoption
including intention to use, perceived ease of use, and perceived usefulness
were not predictive in the study.
After comparing utilizers to non-utilizers, the researchers concluded that physician characteristics most successfully explained the variance in electronic prescribing, as computer experience and information-acquisition style alongside prevalance of medication use best predicted adoption of the system in a primary care setting. Interestingly, the factors that ——
According to the authors, those findings suggest that “the successful integration of electronic prescribing into the day-to-day practice of physicians will require a better understanding of how to present new information in electronic modes to enhance adoption and change physician practice patterns.” Additional study recommendations included offering electronic prescribing applications that “emphasize the value-added benefits — such as prescription refills and access to the current list of dispensed medications — that should improve both practice efficiency and patient safety.”
“Adoption of electronic prescribing is a real challenge — even among early adopters who are usually the most motivated to adopt new technology,” the authors concluded. “Because of the crucial role of early adopters in technology diffusion, thoughtful strategies are needed to ensure adoption and use of electronic prescribing among this crucial group of users.”