Nonalcoholic Fatty Liver Disease Boosts Cardiovascular Risk, But Lacks Management Plan
Growing evidence suggests increased cardiovascular risk in patients with nonalcoholic fatty liver disease (NAFLD) - in particular nonalcoholic steatohepatitis (NASN) - but no data exists to support a specific management approach.
Growing evidence suggests increased cardiovascular risk in patients with nonalcoholic fatty liver disease (NAFLD) — particularly nonalcoholic steatohepatitis (NASH) — but no data exists to support a specific management approach.
Nevertheless, Mary E. Rinella, MD, an associate professor in the gastroenterology and hepatology division at Northwestern University Feinberg School of Medicine, in Chicago, called this an exciting time for hepatologists who are focused on fatty liver disease.
At Digestive Disease Week 2013, held May 18-21, 2013, in Orlando, Fla., Rinella reported on recent studies indicating an association between NAFLD and cardiovascular disorders, including cardiovascular mortality, atherosclerosis, and cardiac structural and functional changes.
According to the World Gastroenterology Organisation’s global guidelines issued in June 2012, the prevalence of NAFLD has doubled in the last 20 years, while the prevalence of other chronic liver diseases has remained stable. Much of the spike may be associated with increases in people’s weight and diabetes, since NAFLD is associated with both. Presently, the prevalence of NAFLD is estimated between 27 percent and 34 percent in the general U.S. population, and 75 percent to 92 percent in the morbidly obese. Most patients with fatty liver have metabolic syndrome and are overweight.
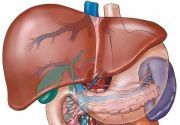
Fatty liver is the most common liver disease, and more patients with the condition are dying from cardiovascular disease than from any other cause, Rinella said.

“While patients with NAFLD have risk factors that are common to those with cardiovascular disease and diabetes, current evidence suggests that NAFLD — specifically NASH — independently affects this and worsens cardiovascular disease,” Rinella added.
Cardiovascular disease occurs in patients with fatty liver “through multiple mechanisms, including but not limited to increased release of pro-inflammatory factors, impaired endothelial function, and atherogenic dyslipidemia,” Rinella said.
With dyslipidema, Rinella said, health care professionals must look beyond the calculated low-density lipoprotein (LDL) cholesterol level to assess whether the LDL is made up of large or small particles.
“People with smaller particles have lower plasma clearance and a greater development of atherosclerotic plaques,” Rinella explained.
Dysfunctional adipose tissue plays a role in both NASH and cardiovascular disease. Additionally, NASH has been associated with procoagulant and inflammatory factors, increased intimal thickening, abnormal left ventricular mass and geometry, diastolic dysfunction, and increased coronary artery calcification, vulnerable plaque, and overt coronary artery disease.
All of that results in significant risk of cardiovascular disease, Rinella noted. But with no data to support a specific approach to managing that risk, she recommended following guidelines from professional societies and to aggressively manage co-morbidities, obesity, diabetes mellitus, and hypertension. While Rinella reported some improvement with weight loss, exercise, and treating the dyslipidemia, she cautioned that dyslipidemia associated with NASH is difficult to treat.
“Future research is needed on the mechanisms effecting hepatic and cardiovascular outcomes,” Rinella said. “And data is needed to determine the cost effectiveness of screening patients.”