Palpatations and Light-Headedness: Another 'Typical' Day
A 73 year-old man presents to the emergency department from his internist's office where he had complained of palpitations and light-headedness that began 4 hours earlier after his daily exercise regimen. He did not appear distressed, but his heart rate was 160 beats per minute. Blood pressure was 140/90. He had no light-headedness at the time, but continued to report palpitations. An ECG was performed.
A 73 year-old man presents to the emergency department from his internist’s office where he had complained of palpitations and light-headedness that began 4 hours earlier after his daily exercise regimen. He did not appear distressed, but his heart rate was 160 beats per minute. Blood pressure was 140/90. He had no light-headedness at the time, but continued to report palpitations. An ECG was performed.
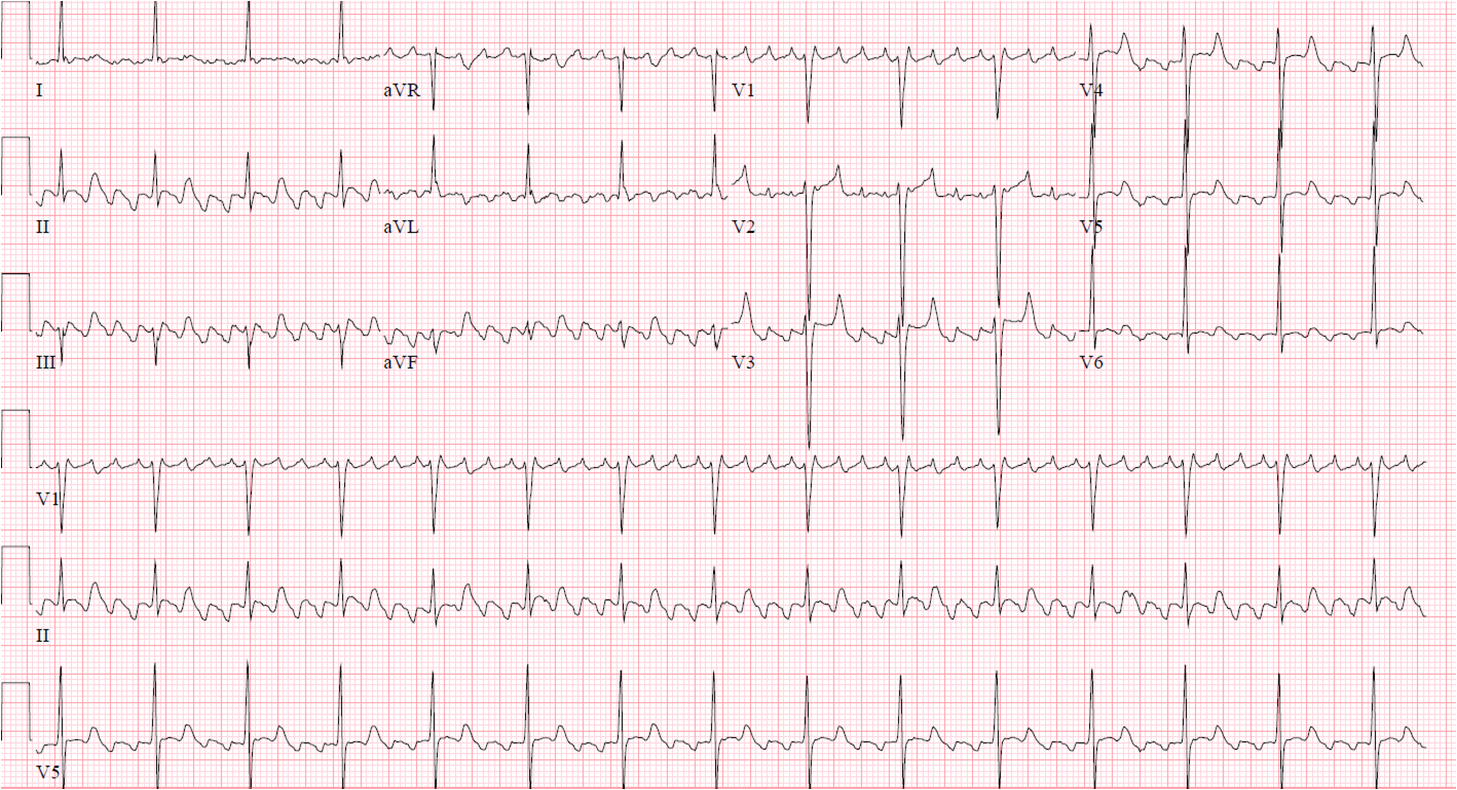
The ECG demonstrates a narrow-complex, regular tachycardia. In leads V1-V3, it looks like there are P waves in front of every QRS and a QRS for every P wave, suggesting this rhythm is sinus tachycardia (ST). The area of the ST segments appears to be abnormal in multiple leads and the T waves inverted inferiorly. Based on these findings, many individuals reviewing this ECG may see this as sinus tachycardia with ischemic changes. However, this ECG is diagnostic of atrial flutter with 2:1 atrioventricular (AV) block.
On further review of the inferior leads, the terminal portion of the QRS seems deeper than usual and similar in morphology to the presumed T wave. Their similarity is due to them both being flutter, or “F”, waves originating in the atrium.
Because the patient was hemodynamically stable, he was started on an esmolol drip and admitted to a telemetry floor. After initiation of the esmolol drip, his heart rate slowed to 90 beats per minute. His follow-up ECG shows more easily identifiable flutter waves with a ratio of 4:1 AV block. AV nodal conduction may also be slowed in narrow complex tachycardias to identify flutter waves with vagal maneuvers or IV adenosine.
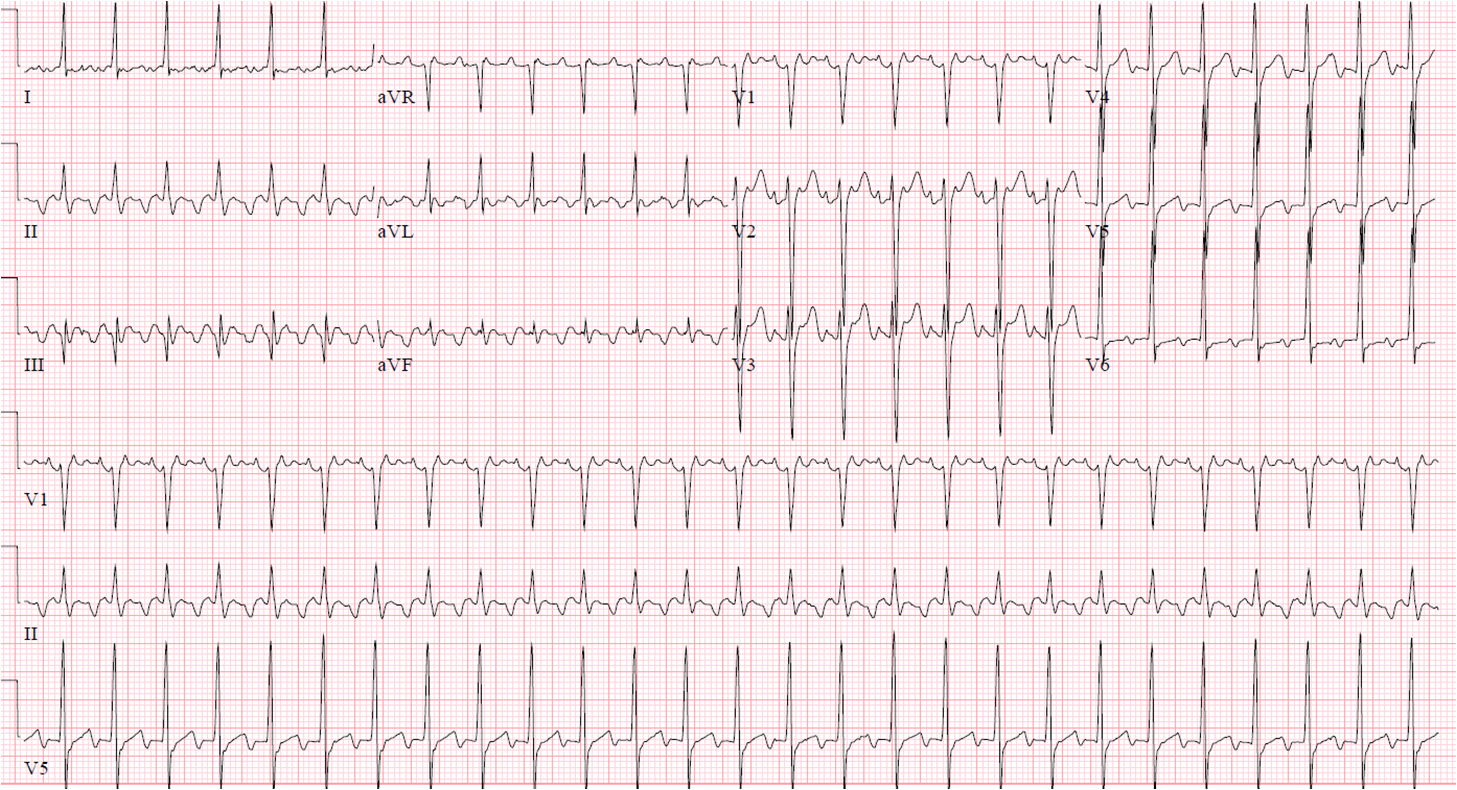
Atrial flutter is characterized by regular atrial undulations occurring at a rate of 240 to 340 beats per minute. Faster flutter rates can be seen in children. Slower flutter rates may be seen in the presence of antiarrhythmic medications or structurally abnormal hearts. Based on morphology of the flutter waves, atrial flutter can be broken down into two categories. The first is called “typical atrial flutter.” Typical atrial flutter is shown in our ECGs. The flutter waves are negatively deflected in the inferior leads (II, III and aVF). The flutter waves will be positive in lead V1. In contrast, “atypical atrial flutter” will often have positive flutter waves in the inferior leads.
QRS complexes can be normal or wide depending on if there is aberrant conduction. Aberrant conduction with wide complexes may be rate-dependent and only be present during rapid ventricular rates. This can cause concern because it looks very similar to sustained ventricular tachycardia.
Atrial flutter does not typically conduct 1:1 due to the very high atrial rates mentioned above. But in situations where the patient is on antiarrhythmics, while still in atrial flutter, the flutter rate may be slowed enough to conduct 1:1.
Otherwise, atrial flutter often conducts with even ratios of 2:1 or 4:1, atria to ventricle. The rhythm may be irregular when a variable block is present with no fixed pattern. On occasion, grouped beating may be present when AV nodal conduction delay is present as in the setting of Wenkebach.
Triggers for atrial flutter are similar to atrial fibrillation and include precipitants like thyrotoxicosis, pulmonary embolism, chronic lung disease, hypertension, myocardial infarction, post-bypass and many other forms of structural heart disease.
The differentiation between typical atrial flutter and atypical atrial flutter is important prognostically. While both flutter moprhologies can be successfully cardioverted to normal sinus rhythm with proper anticoagulation and exclusion of atrial thrombus, typical atrial flutter is successfully treated with 90% long-term success rates by a relatively low risk ablation procedure, performed by an electrophysiologist.
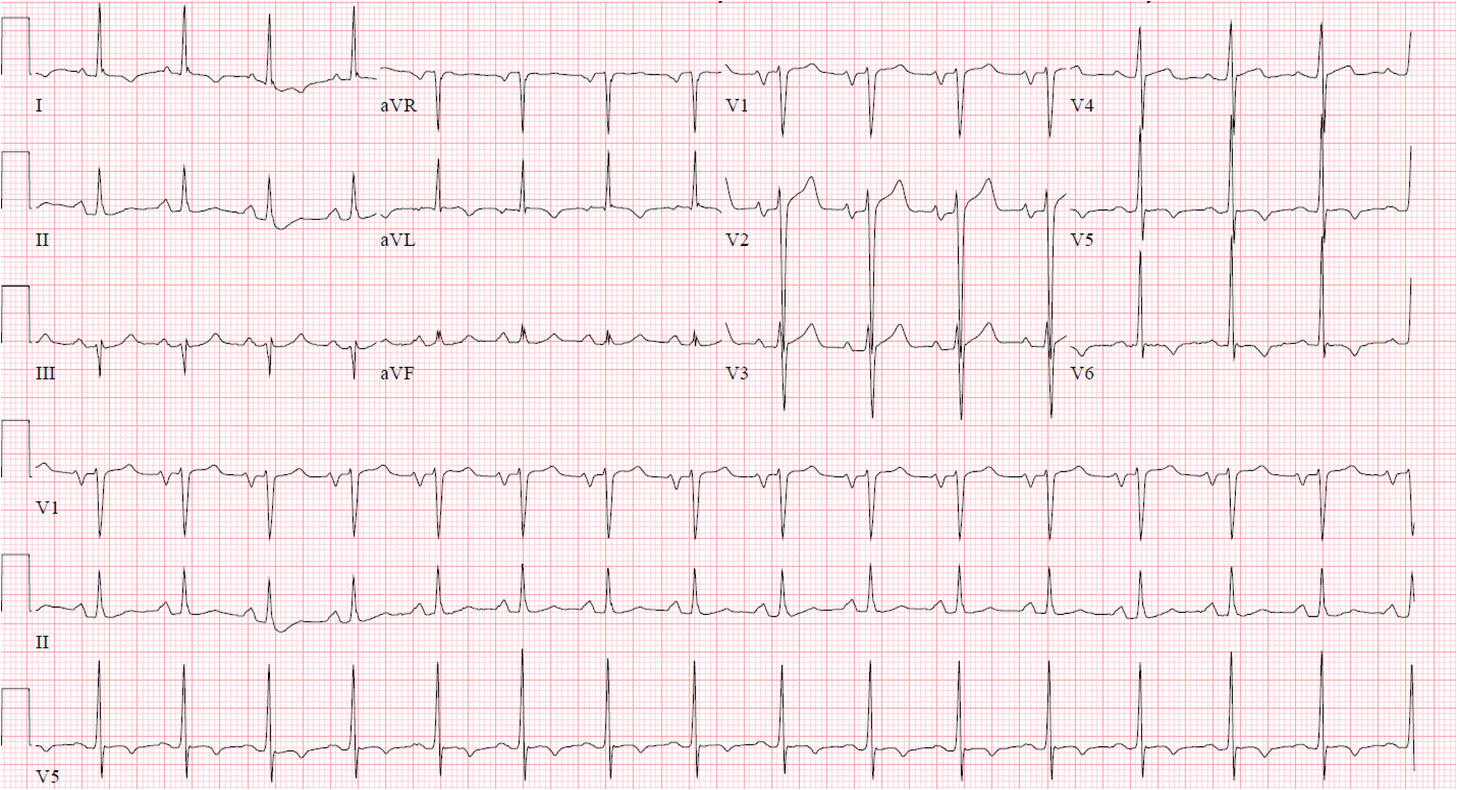
The reproducible nature of typical atrial flutter is due to the predictable anatomical circuit that causes typical atrial flutter. The circuit consists of a counterclockwise, or clockwise, rotation of a reentrant impulse around the tricuspid valve annulus. Ablation can be performed in the area between the IVC and tricuspid annulus known as the isthmus. Following a successful ablation, our patient returned with a more typical ECG.
Braunwald E. et al (2008). Brauwald’s Heart Disease. Philidelphia, PA. Elsevier Saunders.
O’Keefe, H.O. et al. (2008). The Complete Guide to ECGs: A Comprehensive Study Guide to Improve ECG interpretation Skills. Sudbury, MA. Jones and Brtlett Publishers.
Wellens, J.J., Conover M. (2006). The ECG in Emergency Decision Making. St. Louis, MO. Saunders Elsevier.
