Sleep Apnea: Jaw Devices as Good as C-PAP
Mandibular advancement devices and continuous airway pressure are equally effective therapies for reducing blood pressure in patients with obstructive sleep apnea, a study finds.
Mandibular advancement devices (MAD) and continuous airway pressure (CPAP) are equally effective therapies for reducing blood pressure in patients with obstructive sleep apnea, according to a recent analysis. Daniel J. Bratton, PhD, of the Department of Pulmonology, University Hospital in Zurich, Switzerland, and colleagues examined 51 studies and found that there was not a significant difference in how these two devices affected blood pressure (BP). The results of their work appear in the Journal of the American Medical Association on December 1, 2015.
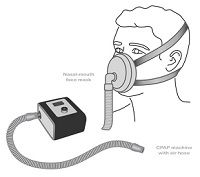
CPAP has been known to be an effective treatment for sleep apnea and “meta-analyses have shown it to be associated with a reduction of about 2mm Hg in BP.” However, many patients cannot tolerate CPAP, and use MADs instead. According to the researchers, “The association of use of MADs with reductions in BP is less clear.” Thus, this study was designed to compare the association of “CPAP vs MADs and vs an inactive control and changes in systolic BP (SBP) and diastolic BP (DBP) in patients with obstructive sleep apnea.”
The researchers identified 51 eligible studies with 4,888 patients, according to their inclusion criteria. Of those, “44 compared CPAP with an inactive control, 3 compared MADs with inactive control, 1 compared CPAP with MADs, and 3 compared CPAP, MADs, and an inactive control.” All of the studies reported SBP, and only one omitted DBP information.
The meta-analysis showed that both CPAP and MADs reduce overall blood pressure, however, CPAP “had a considerably higher probability of having the strongest association with SBP reduction.” However, the researchers concluded “Network meta-analysis did not identify a statistically significant difference between the BP outcomes associated with these therapies.”
This study was limited by the fact that only 2 active treatments, CPAP and MADs were investigated, and by the unavailability of daytime ambulatory BP data. Despite those limitations, the analysis included a large enough number of studies to create reliable models.