Grouping Fibromyalgia Patients by Symptom Incidence, Severity May Improve Treatment Outcomes
Although fibromyalgia lacks an effective standardized treatment, one part of the problem is the condition's diverse constellation of symptoms that include chronic widespread pain, fatigue, and even depression.

Although fibromyalgia lacks an effective standardized treatment, one part of the problem is the condition’s diverse constellation of symptoms that include chronic widespread pain, stiffness, fatigue, and even depression.
Nevertheless, a scientific poster presented March 6, 2014, at the annual meeting of the American Academy of Pain Medicine (AAPM) in Phoenix, AZ, suggests fibromyalgia patients can be grouped into 1 of 4 clusters differentiated by the prevalence and severity of those varied symptom sets, which may better inform therapeutic decisions and yield improved outcomes.
“When a patients comes into the clinic, there is no standardized way to classify the heterogeneity in a way to understand their most bothersome symptom, (as) different physicians have their own ad hoc methods and choices of medications,” lead study author Ann Vincent, MBBS, MD, noted in a press release. “What if we could have a better way to assess patients by classifying the illness from their perspective?”
To test that theory, Vincent and her colleagues from the Mayo Clinic in Rochester, MN, surveyed 1,300 patients who were randomly selected from a clinical fibromyalgia registry that relied on the clinic’s billing records. Using 12 key symptom domains outlined by the Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT) fibromyalgia working group, the poster authors attempted to “cluster the participants according to their response to a comprehensive symptom questionnaire package to identify groups of individuals who reported similar symptom profiles,” Vincent said.
According to the researchers, that questionnaire package included several validated patient outcome instruments representative of the OMERACT symptom domains, such as the Revised Fibromyalgia Impact Questionnaire (FIQ) for multidimensional function and stiffness, the Brief Pain Inventory (BPI) for pain severity, the 30-item Profile of Mood States (POMS) for depression and anxiety, and the Medical Outcomes Study Sleep Scale (MOS) for sleep disturbances.
By applying bottom-up hierarchical clustering to the standardized survey data and then comparing the resulting number of subgroups on a symptom profiles plot and subsequent variable analysis, the poster authors identified 4 clusters of fibromyalgia patients, distinguished by symptom incidence and severity.
The researchers found Cluster 1 patients exhibited the lowest intensity of symptoms such as fatigue, sleep disturbances, pain, stiffness, depression, and anxiety, while Cluster 4 patients had the highest levels of symptom strength. Among the moderate-level clusters, Cluster 3 patients displayed more dyscognition, depression, and anxiety, but less pain, stiffness, dysfunction, poor sleep, and fatigue than Cluster 2 patients.
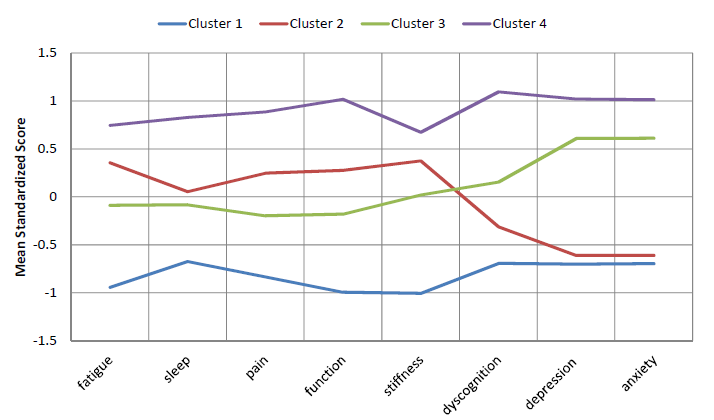
“If a patient’s scores place her in Cluster 1, in which subjects score comparatively low on all symptoms, a clinician might consider initial management with non-pharmacological treatments, such as cognitive-behavior therapy, exercise, physical therapy, and education for self-management of symptoms,” Vincent explained. “Conversely, patients in Cluster 4, marked by higher scores on symptoms, might be preferentially triaged to intensive pain rehabilitation, given that regular outpatient treatment is frequently ineffective in this patient population.”
“Obviously, this needs to be studied,” Vincent added, noting the cluster report was the first of its kind to incorporate a comprehensive spectrum of fibromyalgia symptoms, as recommended by the OMERACT working group. “And this is our next step.”
The study received partial funding from the Mayo Clinic and the National Institutes of Health (NIH).