- Revenue Cycle Management
- COVID-19
- Reimbursement
- Diabetes Awareness Month
- Risk Management
- Patient Retention
- Staffing
- Medical Economics® 100th Anniversary
- Coding and documentation
- Business of Endocrinology
- Telehealth
- Physicians Financial News
- Cybersecurity
- Cardiovascular Clinical Consult
- Locum Tenens, brought to you by LocumLife®
- Weight Management
- Business of Women's Health
- Practice Efficiency
- Finance and Wealth
- EHRs
- Remote Patient Monitoring
- Sponsored Webinars
- Medical Technology
- Billing and collections
- Acute Pain Management
- Exclusive Content
- Value-based Care
- Business of Pediatrics
- Concierge Medicine 2.0 by Castle Connolly Private Health Partners
- Practice Growth
- Concierge Medicine
- Business of Cardiology
- Implementing the Topcon Ocular Telehealth Platform
- Malpractice
- Influenza
- Sexual Health
- Chronic Conditions
- Technology
- Legal and Policy
- Money
- Opinion
- Vaccines
- Practice Management
- Patient Relations
- Careers
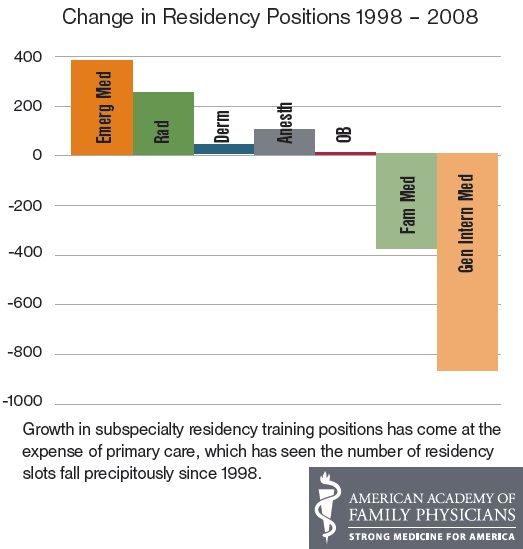
Increased Residency Matches Still Not Enough
Initially, the increased numbers of applicants matching to residency programs seems good, but it probably isn't a large enough increase to keep up with expected demand.
At the highest rate in 30 years, 95% of U.S. medical school seniors matched to residency positions, according to the National Resident Matching Program (NRMP). They made up more than two-thirds of the total applicants who were successfully matched to resident positions.
After applicants were matched, there still remained 1,246 open positions for applicants who hadn’t been matched.
Overall, 81% matched to one of their top three choices. More than 56% of U.S. seniors and half of independent applicants matched to their first choice. Competitive fields, according to the NRMP, were dermatology, orthopaedic surgery, otolaryngology, plastic surgery, radiation oncology, thoracic surgery and vascular surgery.
Despite the good numbers, they might now have been enough considering the looming physician shortage and the additional patients that will be entering the market with health reform.
"While recent efforts have resulted in more residency positions, we remain very concerned that these increases are insufficient to meet the nation’s future health care needs and the looming doctor shortage,” Darrel G. Kirch, MD, president and chief executive officer of the Association of American Medical Colleges, said in a statement.
He added that despite efforts such as increasing enrollment, the industry doesn’t seem on track to avert the 2020 shortage of 90,000 physicians.
The elderly, the poor, rural residents, and the 20 percent of Americans who are already medically underserved will face even greater challenges as a result,” Kirch said. “Because it can take up to 14 years from the time new doctors begin their education until they enter practice, we must begin to act now to avert this shortage.”
In internal medicine, the number of residencies remained virtually unchanged after two years of significant increases. For 2012, 2,941 U.S. medical school seniors matched internal medicine, which is an increase of exactly one from the previous year.
Of that 2,941, roughly 20% to 25% will choose to specialize in general internal medicine, according to ACP. This number is drastically down from 54% in 1998.
"After seeing increases in 2010 and 2011 for the internal medicine residency match for U.S. medical students, we are disappointed that there was not a bigger increase this year," said Virginia L. Hood, MBBS, MPH, FACP, president of American College of Physicians (ACP), in a statement.
The interest in family medicine was also disappointing, according to the American Academy of Family Physicians. Only an additional 18 students were attracted to the specialty and the fill rate (94.5%) barely changed from
2011(94.4%).
“Family medicine is the foundation of health care and is integral to ensuring that Americans get the care they need, when they need it, from the most appropriate health are professional,” said
Glen Stream, MD, MBI, president of the American Academy of Family Physicians
. “That entry into the health care system begins with the family physician.”
Read more:
Top U.S. Research Medical Schools
Top Cities to Live During Med School
