Meeting the challenge of chronic shoulder pain: Treatment
Chronic shoulder pain has a variety of causes, and treatment is multifaceted. Physical therapy typically is the first step; therapy for osteoarthritis (OA) should strike a balance between regaining and maintaining motion and strength and avoiding aggravation of the patient’s condition.
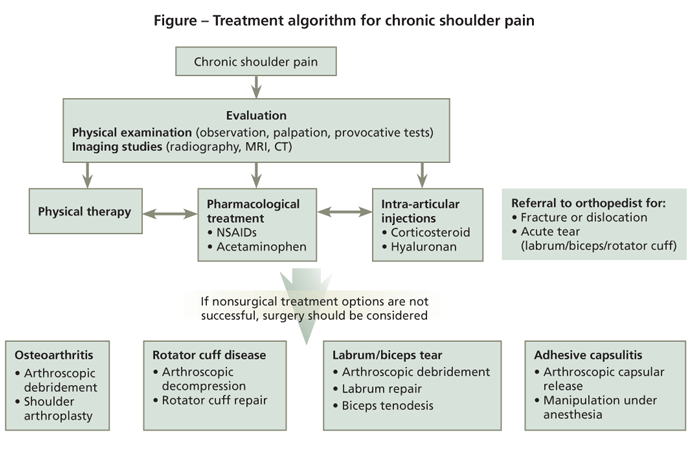
Chronic shoulder pain has a variety of causes-including rotator cuff disorders; osteoarthritis (OA) of the glenohumeral (GH) joint; osteonecrosis; adhesive capsulitis, or frozen shoulder; labral tears; and acromioclavicular (AC) joint pathology-and treatment is multifaceted. Options include physical therapy, pharmacotherapy for pain and inflammation, and local injections (Table and Figure). If
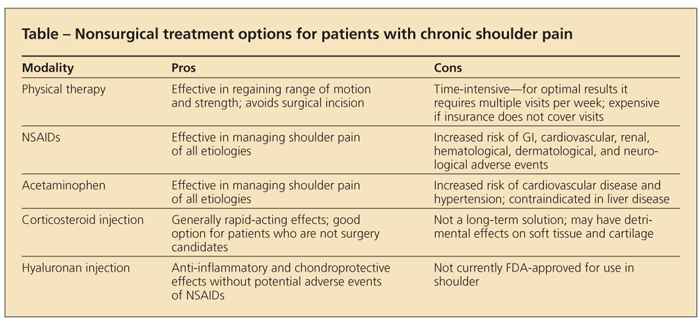
these approaches are not successful, surgical intervention should be considered; surgery is effective in the majority of cases.
This 2-part article provides an update on the latest in chronic shoulder pain diagnosis and management. In the first part (“Meeting the challenge of chronic shoulder pain: The diagnosis,” The Journal of Musculoskeletal Medicine, August 2010, page 317), we focused on making the diagnosis on the basis of the patient history, physical examination, and imaging, offering primary care physicians useful information on which to base treatment and referral decisions. This second part reviews the various nonsurgical and surgical treatment options.
NONSURGICAL
Physical therapy
This typically is the first step in the treatment of patients with chronic shoulder pain, regardless of the cause of symptoms. The type of rehabilitation program often varies with the underlying shoulder pathology.
Physical therapy for OA should strike a balance between regaining and maintaining motion and strength and avoiding aggravation of the patient’s condition. Patients with OA should not be instructed to push through the pain; because structural changes associated with OA may cause a mechanical block to motion, trying to extend this limit is contraindicated.
For those who have pain originating from rotator cuff disease, physical therapy may be very helpful in recovering and maintaining range of motion, increasing rotator cuff strength, and decreasing pain and inflammation. All may be accomplished by performing exercises in the nonimpingement range of motion (below the waist), followed by exercises extending into the provocative range (shoulder level and above).
Patients should carry out individualized stretching programs several times each day to achieve full range of motion. Once range of motion has been restored to at least 80% of normal, strength should be increased through a rotator cuff and scapulothoracic stabilizing program.1 Physical therapists must properly instruct patients in these exercises so that impingement does not occur during strengthening of the rotator cuff.1
Most patients who present with rotator cuff disease respond favorably to a properly designed and executed physical therapy regimen within several weeks of the start of treatment. About two-thirds of patients with rotator cuff disease improve with physical therapy and nonoperative treatment.2
Oral pharmacotherapy
NSAIDs. Oral NSAIDs typically are considered first-line treatment for patients with OA and often are included in the treatment plan for all types of chronic shoulder pain. A few controlled clinical trials have demonstrated the efficacy of NSAIDs and selective cyclooxygenase (COX)-2 inhibitors for patients with shoulder pain.3,4 However, concern has been raised about adverse GI events with conventional NSAIDs and the potential for increasing cardiovascular disease (CVD) risk with both conventional NSAIDs and COX-2–selective agents.5 NSAIDs also carry an increased risk of renal, hematological, dermatological, and neurological adverse effects, which may limit their use.
Consideration of individual patient characteristics is necessary to determine whether NSAIDs or COX-2 inhibitors should be used to manage chronic shoulder pain. The studies that illustrated the adverse effects associated with these agents were conducted in patients who were given the drug for an extended period. A shorter course of treatment (eg, 2 to 4 weeks) should be administered to patients who have shoulder pain to avoid these adverse effects.
Acetaminophen. This agent may be used as an alternative to NSAIDs for pain relief in patients with several types of shoulder pain. A full dose of 1000 mg used up to 4 times a day, for a total of 4000 mg/d, may be effective for pain relief. However, acetaminophen also is associated with an increased risk of CVD, such as hypertension. If acetaminophen is recommended as part of treatment, patients who have liver disease or a high intake of alcohol or who are receiving
anticoagulant therapy should be monitored carefully.
Local therapyCorticosteroid injections. These injections are used frequently in the management of chronic shoulder pain; they may be combined with physical therapy as a first line of treatment. The response usually is quite rapid, and corticosteroid injections can enhance the benefits of physical therapy.
For patients who have rotator cuff disease, many physicians inject a mixture of local anesthetic and short-acting corticosteroid into the subacromial space. Injections for GHOA are administered into the GH joint from an anterior or a posterior approach; these injections may be very effective for patients who are not candidates for surgical treatment.
Hyaluronan injections. Local administration of hyaluronans-large polysaccharide molecules found naturally in the synovial fluid of the joints-may have both chondroprotective and anti-inflammatory effects.6 Although they are not FDA-approved for use in the shoulder, these products have demonstrated efficacy and are approved for use in managing knee OA. More trials are needed to evaluate the use of hyaluronan injections for the management of chronic shoulder pain. However, preliminary data show these medications may provide effective relief for patients with chronic pain without an increased risk of adverse cardiovascular or GI events or other adverse effects.6
SURGICAL
Osteoarthritis (glenohumeral and acromioclavicular)
When chronic shoulder pain is not managed adequately with nonsurgical options, surgical treatment may be considered. Common procedures for GHOA include arthroscopic debridement and shoulder replacement arthroplasty. Techniques include resurfacing arthroplasty, hemiarthroplasty, total shoulder arthroplasty (TSA), and reverse shoulder arthroplasty.
Shoulder arthroplasty for GHOA or osteonecrosis results in improved range of motion and decreased pain in more than 90% of patients.7 TSA, which includes humeral head replacement as well as glenoid resurfacing, provides better functional outcomes than hemiarthroplasty in patients with GHOA.7,8 Some surgeons may perform TSA through a mini-incision less than 2 inches in length, with improved patient cosmesis.9
The presence of a small rotator cuff tear does not negatively influence the outcome of shoulder arthroplasty.8 However, for large rotator cuff tears with associated GHOA, reverse shoulder arthroplasty may be considered. ACOA may be managed arthroscopically, with similar success rates (higher than 90%).10
Rotator cuff disease
Subacromial impingement syndrome (SIS) encompasses several clinical entities, including bursitis, spur formation, and rotator cuff tears. The cause is thought to be a combination of extrinsic factors (eg, bursitis or mechanical wear) and intrinsic factors (eg, tissue degeneration).11 Impingement often is associated with bony changes to the acromion, including spur formation. The spurs can further narrow the subacromial space, increasing the likelihood of contact between the rotator cuff tendons and the acromion and leading to inflammation and pain.11,12 When conservative treatment is not successful in patients with SIS, arthroscopic subacromial decompression may be performed, with success rates higher than 90%.11-13
Rotator cuff tears may be repaired arthroscopically or with an open technique; the goals of surgery are reestablishing the continuity of the cuff mechanism, obtaining a tension-free repair, and creating a smooth acromial surface to limit extrinsic impingement.11 Small rotator cuff tears (less than 3 cm) have much great-er potential to heal than larger tears.14 In most patients, however, even partial healing after rotator cuff repair leads to high rates (higher than 90%) of successful clinical outcomes.12,14,15
Tears of the superior labrum and biceps tendon
The superior labrum (SLAP, superior labrum anterior posterior) and biceps tendon play an important role in GH joint stability. Although degenerative SLAP tears are common in older patients and do not require repair, SLAP tears also may be a source of pain and disability. Nonoperative treatment is successful in about 50% of patients16; however, patients with unsuccessful nonoperative treatment may undergo arthroscopic labral repair; outcomes are successful in more than 90% of patients.17 In severe tears that extend into the long head biceps tendon, biceps tenodesis may be performed.18
Adhesive capsulitis
(frozen shoulder)
Nonoperative management of adhesive capsulitis with physical therapy and stretching is successful in most patients.19 However, surgical treatment may be considered for patients who do not improve. Manipulation under anesthesia avoids a surgical incision but requires an uncontrolled “tearing or rupture” of the capsule. Thus, most surgeons prefer arthroscopic capsular release, which allows for precise release of the capsule with accompanying debridement of inflamed synovial tissue; this procedure is successful in more than 90% of patients.20
References:
References
1. Ferro RT, Jain R, McKeag DB, Escobar R. A nonoperative approach to shoulder impingement syndrome. Sports Med. 2003;3:518-528.
2. Morrison DS, Frogameni AD, Woodworth P. Non-operative treatment of subacromial impingement syndrome. J Bone Joint Surg. 1997;79A:732-737.
3. Petri M, Hufman SL, Waser G, et al. Celecoxib effectively treats patients with acute shoulder tendinitis/bursitis. J Rheumatol. 2004;31:1614-1620.
4. Heller B, Tarricone R. Oxaprozin versus diclofenac in NSAID-refractory periarthritis pain of the shoulder. Curr Med Res Opin. 2004;20:1279-1290.
5. Akarca US. Gastrointestinal effects of selective and non-selective non-steroidal anti-inflammatory drugs. Curr Pharm Des. 2005;11:1779-1793.
6. Blaine T, Moskowitz R, Udell J, et al. Treatment of persistent shoulder pain with sodium hyaluronate: a randomized, controlled trial. A multicenter study. J Bone Joint Surg . 2008;90A:970-979.
7. Iannotti JP, Norris TP. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg. 2003;85A:251-258.
8. Bryant D, Litchfield R, Sandow M, et al. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder: a systematic review and meta-analysis. J Bone Joint Surg. 2005;87A:1947-1956.
9. Blaine T, Voloshin I, Setter K, Bigliani LU. Minimally invasive approach for shoulder arthroplasty. In: Scuderi GR, Tria AJ Jr, Berger RA, eds. MIS Techniques in Orthopedics. New York: Springer Science+Business Media, Inc; 2006:45-70.
10. Levine WN, Soong M, Ahmad C, et al. Arthroscopic distal clavicle resection: a comparison of bursal and direct approaches. Arthroscopy. 2006;22:516-520.
11. Neer CS 2nd. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg. 1972;54A:41-50.
12. Blaine TA, Miller S. Subacromial decompression/rotator cuff repair. In: Blaine TA, ed. Shoulder Arthroscopy. Rosemont, IL: American Academy of Orthopaedic Surgeons. Monograph Series. 2006.
13. Björnsson H, Norlin R, Knutsson A, Adolfsson L. Fewer rotator cuff tears fifteen years after arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2010;19:111-115.
14. Bishop J, Klepps S, Lo IK, et al. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15:290-299.
15. Miller NL, Wu X, Tantau R, et al. Open versus two forms of arthroscopic rotator cuff repair. Clin Orthop Relat Res. 2009;467:966-978.
16. Edwards SL, Lee JA, Bell JE, et al. Nonoperative treatment of superior labrum anterior posterior tears: improvements in pain, function, and quality of life. Am J Sports Med. 2010;38:1456-1461.
17. Kim SH, Ha KI, Kim SH, Choi HJ. Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg. 2002;84A:981-985.
18. Koh KH, Ahn JH, Kim SM, Yoo JC. Treatment of biceps tendon lesions in the setting of rotator cuff tears: prospective cohort study of tenotomy versus tenodesis. Am J Sports Med. 2010;38:1584-1590.
19. Levine WN, Kashyap CP, Bak SF, et al. Nonoperative management of idiopathic adhesive capsulitis. J Shoulder Elbow Surg. 2007;16:569-573.
20. Elhassan B, Ozbaydar M, Massimini D, et al. Arthroscopic capsular release for refractory shoulder stiffness: a critical analysis of effectiveness in specific etiologies. J Shoulder Elbow Surg. 2010;19:580-587.