Studies Say Vitamin D Deficiency Doesn't Increase Odds of RA, But May Worsen OA Symptoms
Though previous reports have described a link between vitamin D deficiency and an increased risk of rheumatoid arthritis (RA) development, a trio of studies has now offered clinical support to the contrary belief.

In light of the growing evidence on immunoregulatory properties of vitamin D in suppressing autoimmunity, previous reports have described a link between vitamin D deficiency and an increased risk of rheumatoid arthritis (RA) development. However, a trio of studies presented at the American College of Rheumatology 2013 Annual Meeting in San Diego, CA, has now offered clinical support to the contrary belief.
In the first study, which was presented during a poster session on the human etiology and pathogenesis of RA, Jonida Cote, DO, and colleagues from the Division of Rheumatology at Geisinger Health System in Danville, PA, matched 270 incident RA patients to 1,341 control subjects by age and gender using electronic health records (EHR) in order to evaluate the association of vitamin D levels with RA.
According to the researchers, “vitamin D levels were treated both as continuous and categorical; we used <30 IU as the primary cutoff, but also used <20 IU to investigate the RA association with severe vitamin D deficiency.” Among all RA patients and matched controls, the median age was 62.4 years old and the median vitamin D level was 31 IU.
At the conclusion of their analysis — which adjusted for obesity and current smoking status and was powered at 82% to detect an odds ratio (OR) of 1.5 — Cote and her co-authors determined that “low vitamin D level was not associated with increased odds for incident RA,” as both rheumatoid factor-positive patients and rheumatoid factor-negative patients with vitamin D levels below 30 IU were not at an increased risk of developing RA (Table 1).
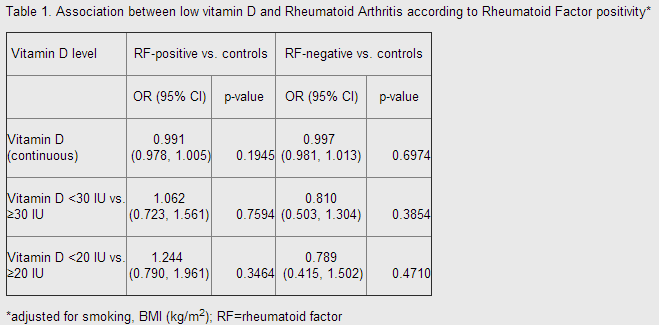
However, Cote said during the poster session that she was puzzled by the fact that male patients with vitamin D levels below 20 IU were less likely to develop RA compared to their male counterparts with higher vitamin D levels of up to 30 IU, though she attributed those peculiar results to the small size of the male RA case cohort (n= 45).
In the second study entitled “Effect of Vitamin D on Early Rheumatoid Arthritis: A Retrospective Cohort Analysis,” which was presented during a poster session about RA disease course predictors, Faye A. H. Cooles, MBChB, MRCP, of the Musculoskeletal Research Group at Newcastle University and colleagues examined the effect that serum 25-hydroxy vitamin D (25OHD) levels had on disease activity and general health scores, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), tender and swollen joint counts, and autoantibody status in 453 patients with early-stage RA and a median symptom duration of 16 weeks.
According to Cooles and her research team, statistical analyses determined that there was no significant association between 25OHD levels and those disease-related measures — even among the 73 patients who had been diagnosed with persistent RA. Therefore, the researchers concluded that 25OHD “does not impact disease activity parameters in early disease.”
Nevertheless, low vitamin D levels may play a substantial role in osteoarthritis (OA), as Cooles and her co-authors demonstrated considerably longer disease-related symptom duration and a “significant inverse relationship between (general health scores) and serum 25OHD” in the 58 OA patients included in their study. However, the authors noted that the impact of 25OHD on the other parameters described in their poster was just as non-significant in OA patients as it was in those with RA.
But the third study presented during a poster session on RA comorbidities did offer evidence of 25OHD levels correlating with an RA diagnosis among patients who are experiencing the early development stage of the rheumatic disease.
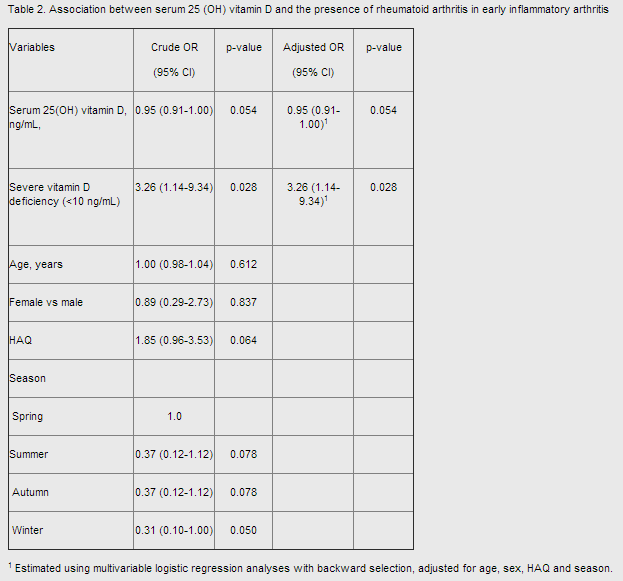
For their “Vitamin D Deficiency in Patients with Early Inflammatory Arthritis” poster, Seung-Geun Lee of the Department of Internal Medicine at the Pusan National University School of Medicine and researchers in Busan, South Korea, compared serum 25OHD levels in 101 patients with early inflammatory arthritis (EIA) and symptom duration of at least 6 months to those in 101 age- and gender-matched healthy control subjects.
Although there was no significant difference in serum 25OHD levels between the EIA patients and the non-RA subjects, the investigators ultimately discovered that “vitamin D deficiency contributed to the presence of RA in EIA patients, (and) severe vitamin deficiency was significantly associated with the diagnosis of RA” (Table 2).
Despite all of the researchers' evidence-based conclusions, Cooles and her co-authors wrote that “larger scale studies are needed to validate our preliminary findings in early arthritis.”