Interventional Pain Management: Let's Abandon the Safe Triangle
Using the widely taught 'safe triangle' approach to transforaminal epidural injections can paralyze patients. There's a safer way.
In 2001, a delightful, active, slightly older than middle-aged woman came to see me in the office of my pain management practice in Chicago.
She had been down in Florida with her husband, an ex-Marine, and was on a boat ride when it hit a wave and she fell.
She had a compression fracture which slowly healed. However, she also suffered from severe chronic pain from a nerve passing by that fracture that became inflamed.
I was confident I could help her.
I have helped so many others with similar conditions by doing a pain-blocking injection near the nerve as it comes out the intervertebral foramen.
The injection consists of local anesthetic and a crystallized steroid.
I had learned how to do these transforaminal injections and nerve blocks from the leading physicians in the field at cadaver workshops. It was truly a miraculous procedure and I was helping people I had never been able to help before.
I performed the procedure using the technique I had been taught utilizing live fluoroscopy.
I used the standard-of-care approach, the "safe triangle".
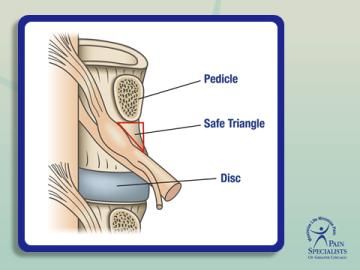
This approach had recently been developed, defined as placing the needle in a specific area of the intervertebral foramen, the superior and anterior aspect of the foramen, to avoid hitting the nerve, the disc, or the thecal sac.
Everything seemed to go well: The contrast flow was perfect, outlining the exiting nerve root and flowing into the epidural space.
I injected the medications, confident of success.
But it had not gone well at all.
Before finishing my dictation I was alerted that the patient could not move her legs and could not be transferred to the gurney.
She never moved them again.
was confirmed by an MRI.
The procedure I performed had caused an infarction, a stroke, of her spinal cord. The damage
Awareness of what I had done to this patient slowly dawned upon me over the next 24 hours.
I was filled with sadness, guilt, but also anger.
How could this procedure which I had been taught and which supposedly had never been associated with this complication, and which was called "safe" lead to this almost unfathomable outcome?
I visited my patient at The Rehab Institute of Chicago after clinic every day, full of remorse for this kind, lively woman and her family.
After considering all options to provide her some financial aid it became clear that the only path was for her to sue me.
I felt she and her husband would have difficulty doing that because of their decency and, in my opinion, because they were members of their more selfless generation. So I told her privately that it was her only course of action.
I told her that although I believed I had done nothing wrong, in the current medico-legal climate, the only way to get money from the insurance company was for a doctor to be sued.
Reluctantly, she agreed.
As I prepared for the malpractice trial and studied the vascular anatomy of the foramen, it became clear to me and to the expert who defended me, Frank Falco, MD, that this recently developed, "standard of care", technique for performing transforaminal injections was/is fatally flawed.
Simply put, the originators of the "safe triangle" did not account for or show any awareness of the presence of the vascular supply to the spinal cord within the foramen.
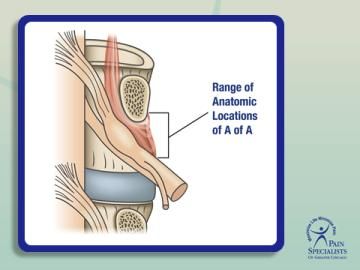
This singular artery, the Artery of Adamkiewicz, can be found in any of the thoracic or lumbar foramina but it is always in the same location within the foramen. Its location in the foramen coincides with the exact location the safe triangle technique teaches doctors to place their needles.
This means that the blood flow to the spinal cord is endangered each and every time this procedure is performed using the "safe triangle”.
This is a totally unnecessary and unacceptable risk.
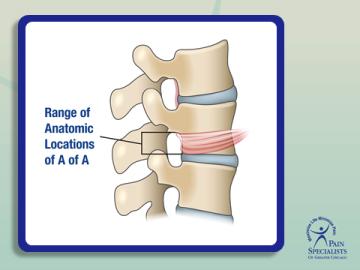
The illustrations below show the anatomy involved. In the first x-ray from an actual procedure, note the safe triangle technique from a lateral view. The needle is below the pedicle connecting the front and back of the vertebra in the superior and anterior aspect of the foramen In the second illustration, note the location of the safe triangle just below the pedicle and above the nerve. In the third illustration, note the locations the artery has been found on anatomic studies graphically shown to correspond to the same area as the safe triangle. In the fourth illustration, which corresponds to the same view as the first x-ray, note the locations of the artery in the superior and anterior aspect of the foramen- the same location the safe triangle places the needle

Later, at the trial, I was astonished to find out that the two expert witnesses for the patient suing me were both doctors heavily involved in the development and the promulgation of this technique, both of whom I had learned from in person.
I was further distressed to observe these experts manufacture theories that blamed my performance of the procedure, not the procedure itself. I was consumed with guilt because of the outcome but I knew that I had performed the procedure exactly as it was taught.
Unfortunately, the way I was taught was the fatally flawed “safe triangle” technique and my patient had paid the price.
Obviously, the “safe triangle” is anything but safe.
But there is an alternative approach that salvages this truly amazing pain-relieving procedure.
The transforaminal injection can be performed in the inferior foramen, posterior to the disc, and as far as possible from the artery.
Although many physicians are aware of this issue and do perform the procedure away from the safe triangle, it is probably not the majority of them.
Performing the procedure away from the "safe triangle" maintains and possibly improves the effectiveness of the procedure since the medications are deposited closer to disc/nerve interface--the spot where most radicular pain originates.
But, more importantly, doing the procedure in this manner makes it safe. I have used that approach and performed over 100,000 of these procedures since that fateful day in 2001 without a complication.
The x-ray below shows this technique, the true "safe" area of the foramen, below the nerve as far as possible from the locations of the atery.

Over the years, with the help of Rinoo Shah, MD, clinical professor in the Louisiana State University pain managment fellowship program, I have devoted time and energy to alerting others of this risk so that the "safe triangle" approach will be abandoned and replaced by the safer approach below the nerve away from the artery. We co-authored an article on the topic in Pain Management in 2010. Shah has gone on to write more articles on the topic.
With the help of other like-minded experts in the field, I have written and co-authored other articles and 3 book chapters on this issue.
Last November, I presented this information in front of the US Food and Drug Administration's advisory group on spinal injections and particulate steroids.
I have presented at national and state level meetings in an attempt to change the standard of care. In spite of what appears blindingly obvious to me and others, the teaching and use of the “safe triangle” approach persists.
Frank Falco, past ASIPP president and Director of Temple University Hospital’s Pain Management Fellowship Program, co-authored the original case report describing the dangers of the "safe triangle".
Lax Manchikanti, MD, founder and CEO of ASIPP, feels the issue is gravely important and has given me the ability to present this information to a national audience.
But I remain frustrated by the glacially slow pace of change in the standard of care.
The "safe triangle" approach is ingrained as the "standard of care" secondary to its continued teaching at workshops and in residencies and fellowships.
As a consequence, cases of paraplegia continue to accrue.
There are now 18 cases in the literature, I am aware of 16 others through expert witness work, and my good friend, Gabor Racz, MD, estimates that he has reviewed 50 cases.
It is tragic to read the depositions of the patients who are looking for pain relief and trying to avoid more invasive procedures who are paralyzed in an instant, suffering severe transient back pain from the infarct itself and then becoming aware they can no longer move their legs.
It is almost as devastating to read the depositions of the physicians who are in denial, traumatized that they have rendered a patient paralyzed by a procedure they had been led to believe was "safe" based on the very name of the technique.
However, another type of tragedy unfolds when one reads the depositions of the "expert" witnesses for the paralyzed patients who strive to impugn the care of the very physicians they have taught at workshops.
It is hard to imagine what goes through their minds.
It is hard to believe they can deal with the cognitive dissonance that must be associated with profiting financially in this manner.
It is even harder to believe and morally repugnant that these experts, aware of the risks, continue to perform these injections and teach others utilizing this fatally flawed technique.
As soon as the first case report of paralysis appeared, the inventors and purveyors of this dangerous technique should have stripped the procedure down to its basics and deconstructed it.
They should have searched for a root cause as we have discovered.
Instead, they have recommended technique modifications which have not protected the patient.
Not unexpectedly, each one of these modifications has been shown to fail to prevent paraplegia.
All are based on the false premise that there only one mechansm of injury, the embolisation of steoid particles leading to occlusion of blood vessels.
That has been proven wrong as there is another mechanism of injury, direct damage to the artery itself.
The experts' newest “solution” to prevent paraplegia is another technique modification, the use of non-particulate steroids instead of the steroids in crystal form.
Again, this technique modification will successfully reduce cases paralegia on the one condition that the only mechanism of injury is embolisation of particulates- but that has been proven to not be the only mechanism of injury. Therefore, this "solution" wlll not prevent paraplega.
In actuality,this is a hypothesis, not a proven fact, and is based on minimal as well as tangential evdence.
It is not a solution to the problem of paraplegia. In essence, using non-particulate steroids instead of particulate steroids wll be a large scale prospective study on the American public as there is no real proof this type of steroid is safer. At the current tme,
The innocent an unknowing participants in this ill-advised study will be patients coming to physicians for transforaminal injections.
Tragically, non-particulate steroids will not protect patients either and paraplegia cases will continue to occur.
The failure of these technique modifications is related to the fact that there is another mechanism of injury. It has been conclusively shown that there is trauma to the artery by the needle causing intimal flaps, clot, and vasospasm which causes occlusion, blockage of blood flow, and the infarct.
The mechanism of injury is not simply secondary to the embolism of steroid particulates alone as which is the postulate all of these failed strategies are based on.
In the worse tradition of unintended consequences, a wholesale transition to non-particulate steroids will not reduce the incidence of paraplegia.
In all actuality, the incidence of paraplegia will be more likely to increase as patients receive lower quality and shorter duration of relief as non-particulate steroids are clearly not as effective.
Conversely, this will in turn lead to more needles being placed in proximity to the artery and more cases of paraplegia secondary to local trauma with the resultant sequelae secondary to injury to the artery.
Additionally, another tragic unintended consequence will be more patients opting for surgery and narcotic pain medication use with their well documented risks.
Transforaminal epidural steroid injections are remarkably effective and are life-changing in their ability to reduce different types of pain related to the spine.
However, using the “safe triangle” approach to this procedure carries unacceptable risks. It has changed my patient’s life forever.
It is still happening to other patients.
I cannot rest until this technique, the "safe triangle" approach to transforaminal epidural ster injection, is relegated to the dustbin of medical history secondary to its unacceptable and unnecessary risk of such a tragic and irreversible complication.