MRI Patterns Decipher Between Multiple Sclerosis and Vanishing White Matter Disease
New evidence has made it easier to differentiate between multiple sclerosis and vanishing white matter disease, conditions that can show considerable similarities.
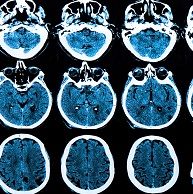
New evidence has made it easier to differentiate between multiple sclerosis (MS) and vanishing white matter disease (VWM) — conditions that can show considerable similarities.
According to the presentation at the American Academy of Neurology in Washington, DC, diagnosing primary and secondary progressive multiple already presents a challenge because the signs — like large and confluent lesions and multiple cavitary lesions – are rarely shown on a brain MRI. However, the comparable symptoms with VRM can cause a misdiagnosis.
“It is important to identify specific MRI findings that can be relevant diagnostic tools,” the authors wrote.
Lead author Xavier Ayrignac, of the Department of Neurology in Centre Hospitalier Universitaire de Montpellier in France, and his colleagues evaluated 14 MS and 14 VWM patients to find key differences between their brain scans. The candidate pool consisted of a female to male ratio of 7:7 for MS and 10:4 for VWM as well as an average age of onset of 39.9 for MS and 35.1 for WVM.
“In this context, the diagnosis of Multiple sclerosis can be difficult and a diagnosis of Vanishing White Matter should be considered,” Ayrignac and his team determined.
When cavitary lesions show up on the MRI, it becomes more challenging to decipher between the central nervous system diseases. The researchers focused on specific features including regional atrophy, white matter and gray matter hyperintensities location and type, and posterior fossa involvement along with middle cerebellar peduncle and cerebellar white matter lesions.
While similar results were indicated between the MS and VWM patients — like focal atrophy, basal ganglia atrophy, and corpus callosum atrophy – the investigators found important individualized characteristics for the diseases:
- Cerebellum atrophy: 8 (57%) MS patients, 13 (93%) VWM patients
- Topography of the lesions (thalamus): 10 (71%) MS patients, 1 (7%) VWM patients
- Topography of the lesions (midbrain): 11 (79%) MS patients, 4 (29%) VWM patients
- Extensive juxtacortical lesions: 7 (50%) MS patients, 14 (100%) VWM patients
- Ovoid perpendicular to the ventricle: 14 (100%) MS patients, 0 VWM patients
- Corpus callosum extensive: 9 (64%) MS patients, 14 (100%) VWM patients
- Extensive lesions (external capsule): 4 (29%) MS patients, 12 (86%) VWM patients
- Perivascular cavitary lesions: 10/12 (83%) MS patients, 1/6 (17%) VWM patients
- Infratentorial symmetrical: 0 MS patients, 6/12 (50%) VWM patients
- Fluid like cavitary lesions: 3 (21%) MS patients, 9 (64%) VWM patients
“Nevertheless, our results suggest that the analysis of characteristics of MRI findings including topography and morphology of the lesions is of major diagnosis importance for the differential diagnosis of these 2 disorders,” the team concluded.