Both Risks and Costs Are Doubled in Lupus Pregnancies
ACR2013: Retrospective analysis of more than 10,000 pregnancies documents increased risks for hypertension, preeclampsia, preterm delivery and stillbirths among women with SLE.
A retrospective analysis of more than 10,700 pregnancies among women with and without systemic lupus erythematosus (SLE) shows doubled risks for hypertension, preeclampsia, preterm delivery, and stillbirths among women who have SLE.
The analysis of a US administrative healthcare claims database also finds a more than 16-fold occurrence of nephritis in SLE pregnancies.
The review, presented at the 2013 annual meeting of the American College of Rheumatology in San Diego, analyzed data from 1,721 SLE pregnancies and 8,605 non-SLE pregnancies from 2006 to 2012.
The report tracked live births, miscarriage, and first-or second trimester ultrasound, using records for at least two different days among women (mean age 31) matched by date, geography, and insurance plan type.
“Data from this large US database shows us that the complications of lupus pregnancy are very real and that the costs of managing a lupus pregnancy are huge,” said Michelle Petri MD in an interview at the ACR meeting.
“It costs about $20,000 to manage a lupus pregnancy compared with $10,000 for a non-lupus pregnancy "So it’s double the cost. And we’re still having problems with the outcomes,” added Petri, who is professor of medicine and director of the Johns Hopkins Lupus Center in Baltimore. “I hope the new health care law will make it possible for women with pre-existing conditions like lupus to actually get health insurance. Right now, it’s very difficult to see how we are going to reduce the costs of lupus pregnancy.”
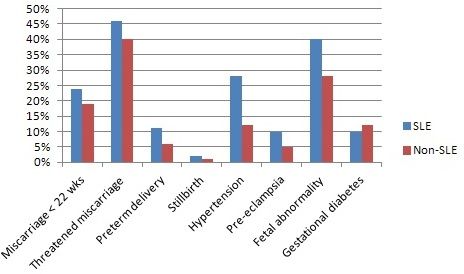
For SLE pregnancies compared with those of unaffected women, Petri’s team found:
• Miscarriages before 22 weeks: 23.9% (SLE pregnancies) vs 19% (non-SLE)
• Threatened abortion/premature labor without delivery: 46.0% vs 39.8%
• Hypertension: 28.4% vs 12.4%
• Preeclampsia: 9.9% vs 4.5%
• Preterm delivery (at 22-35 weeks): 11.4% vs 5.9%
• Stillbirths: 2.4% vs 1.3%
• Fetal complications: 68.9% vs 64.1%
• ICD code for known/suspected fetal abnormality affecting management of the mother: 39.7% vs 28.0%
• In contrast, gestational diabetes: 9.8% vs 11.9%
"Our report has some very important messages for clinicians,” Petri said. “For example, hydroxychloroquine was used by fewer than 50% of the pregnant women, even though we now know it can prevent lupus flares in pregnancy and neonatal lupus.”
“In addition, there were very few visits to rheumatologists on average during pregnancy and that may be one reason drug that utilization was not optimized during pregnancy,” she added. “In my practice, a pregnant woman will see me every 4 to 6 weeks, so I found these data shocking. But they are real; they reflect what is happening.”