Caring for Caregivers
Caregivers are a rheumatologist's most important allies. Learn the warning signs of caregiver burnout and how to combat the symptoms. Remember: their health is prerequisite to patient care.
Of course, you already know that rheumatology patients have some of the highest risks for mental health complications, but you may be unaware about the extraordinarily high risks to their caregivers. There are legions of vulnerable caregivers in this country, with 43.5 million people in the United Sates providing care to chronically ill family members and friends annually. Nearly every caregiver for patients with chronic inflammatory diseases experiences increased anxiety and stress in relation to their caregiving role. A total 98% of respondents in 1 study1 and 80% of caregivers in another study2 reported they feel burdened by their role. The caregiving burden can be especially taxing for patients with chronic pain where research suggests3 that 96% of those caregivers experience sadness, 65% report sleep disturbances, and 75% report that they have had to abandon or change other responsibilities. That same study reported that nearly 1 quarter of caregivers appraised their own health to be worsening. In the same ways that risk for burnout applies to you in your professional role, caregivers also experience compassion fatigue and then their experience directly impacts your patients.
Maddy Pontius, BA

For rheumatoid arthritis (RA) patients, there is a significant relationship4 between the perception of burdensomeness and increased pain intensity, functional limitations, depressive symptoms, and anxiety. In 1 study of RA patients, physical disability actually increased as reported caregiver pessimism and hopelessness increased. Patients with burned out caregivers5 are at a greater risk for falling, developing preventable disease complications, and experiencing declines in functional abilities. My own professional association, the American Psychological Association, went so far as to say “… the health and well-being of family caregivers – and the subsequent ability to assist their care recipients – is a public and mental health priority.”
For all of these reasons, a partnership between rheumatologists and caregivers is imperative. Obviously, patients rely on their caregivers for assistance with daily activities, navigating the healthcare system, and communicating with healthcare professionals. In this way, your patient’s caregiver,6 specifically their attitudes and agreement your treatment plans, will inevitably affect patient care. Working to establish a collaborative, respectful relationship is related to better outcomes all around, but where do you start?
If you don’t already know something about a patient’s support system, ask about their network and the caregivers in their lives. Make a point to retain your patient-centered model of care while also recognizing the value and importance of the caregivers; perhaps consider inviting them to an upcoming appointment. With the relevant HIPAA signatures in hand, you can broker a discussion to ensure there is a common understanding of your patient’s condition, treatment, and their wishes between you, the patient, and their caregiver(s). In this way, you are actually promoting autonomous decision-making. Of course, managing your patient’s privacy is an ongoing priority so you will routinely assess your patient’s preferences regarding the nature and degree of caregiver involvement, always listening for problematic relationship dynamics (see our column on responding to interpersonal violence in the home). Joint meetings won’t completely replace individual meetings where patient care is delivered and confidential matters can be addressed, but these joint meetings are 1 of your most powerful clinical tools.
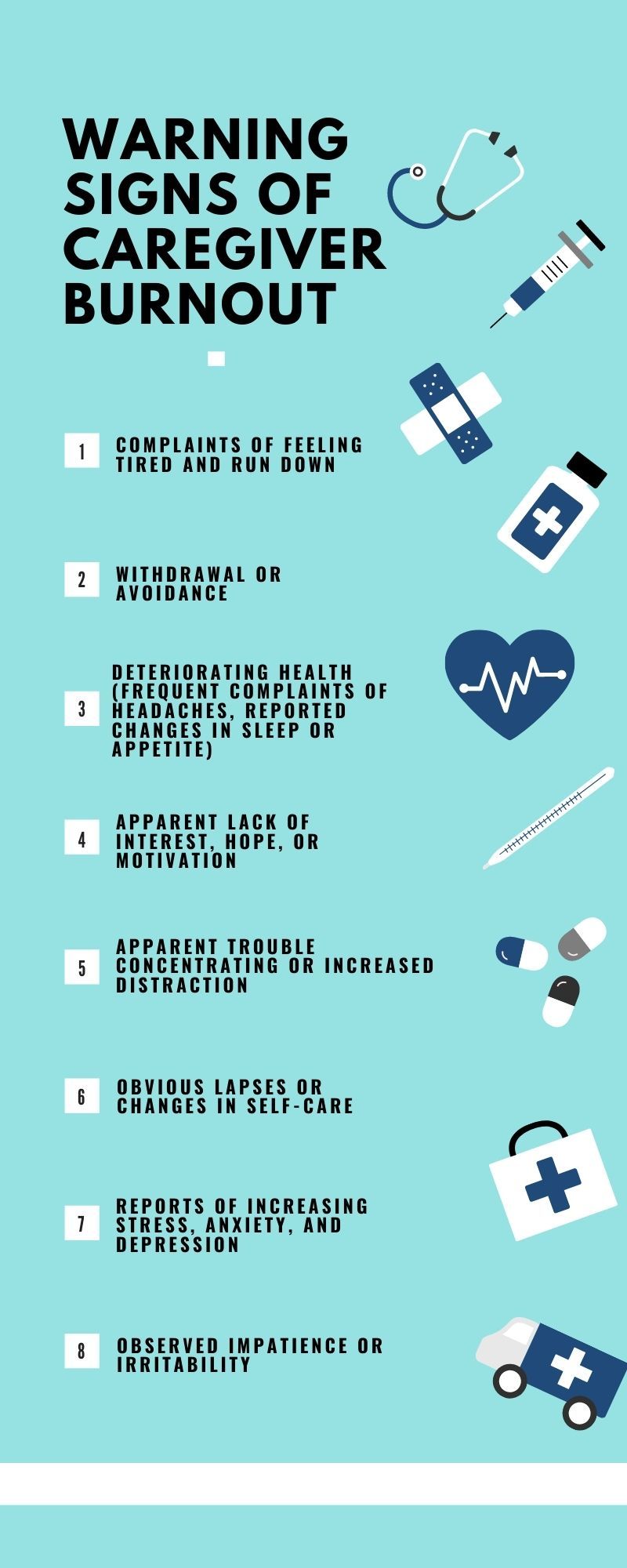
Importantly, as you recognize caregiver distress (see below) remember that your only responsibility is to provide appropriate referrals so that you can continue to prioritize your patients’ health. In the cases of exploitation or abuse, you should be prepared to make an emergent referral to social services or safehouses, but you can assume that you will mostly be called on to “prescribe” self-care and to remind caregivers to be proactive with their own health and wellbeing. As a matter of routine, you can establish referrals between caregivers and local disease-specific social networks or support groups. More than anything, remember that you have everything in common with these caregivers and they are your most important allies. Their health is prerequisite to patient care.
References:
1. Al Sawah, S., Daly, R.P., Foster, S.A., Naegeli, A.N., Benjamin, K., Doll, H., Bond, G., Moshkovich, O., & Alarcón, G.S. (2017). The caregiver burden in lupus: findings from UNVEIL, a national online lupus survey in the United States. Lupus, 26(1), 54-61. https://doi.org/10.1177%2F0961203316651743
2. Ru, J., Ma, J., Niu, H., Chen, Y., Li, L., Liu, Y., Li, X., Lian, F., & Wang, X. (2018). Burden and depression in caregivers of patients with rheumatoid arthritis in China. International Journal of Rheumatic Diseases, 608-613. https://onlinelibrary.wiley.com/doi/full/10.1111/1756-185X.13397
3. Ojeda, B., Salazar, A., Dueñas, M., Torres, L. M., Micó, J. A., & Failde, I. (2014). The impact of chronic pain: The perspective of patients, relatives, and caregivers. Families, Systems, & Health, 32(4), 399–407. https://doi.org/10.1037/fsh0000069
4. Beckham, J.C., Burker, E.J., Rice, J.R., & Talton, S.L. (2010). Patient Predictors of Caregiver Burden, Optimism, and Pessimism in Rheumatoid Arthritis. Behavioral Medicine, 20(4), 171-178. https://doi.org/10.1080/08964289.1995.9933734
5. American Psychological Association. (2011). Family Caregiver Well-Being is Important to Care Recipient Health. Retrieved from https://www.apa.org/pi/about/publications/caregivers/faq/well-being
6. National Association of Chronic Disease Directors. (2010). CDC Seeks to Protect Health of Family Caregivers. Retrieved from https://www.chronicdisease.org/resource/resmgr/healthy_aging_critical_issues_brief/ha_cib_healthoffamilycaregiv.pdf