Clinical management of muscle strains and tears
Muscle strains are most common in the hamstring, gastrocnemius, soleus, and quadriceps strains, as well as the lumbar and thigh adductor. This image-rich review covers imaging, treatment, and prevention.
Muscle strains and tears are injuries to a muscle or tendon that occur when the muscle is stretched too far too fast. These injuries are common in athletes, especially hamstring, gastrocnemius and soleus, quadriceps, lumbar, and adductor strains; complete tears are less common. Most patients with strains present after an acute onset of pain during activity. Physical examination may reveal local swelling or ecchymosis; palpation usually reveals localized tenderness over the myotendinous junction. Radiographs may demonstrate soft tissue swelling; MRI is occasionally helpful for local injury. Acute management generally includes rest, ice, compression, elevation, and use of NSAIDs. An exercise program should be instituted. Flexible, strong, and warmed-up muscles are the key to strain rehabilitation and injury prevention. (J Musculoskel Med. 2008;25:526-532)
Skeletal muscle injuries are found frequently in all types of athletes, young and old, recreational and professional. This category of injury may include strains, tears, delayed onset muscle soreness, and contusions. Here we focus on strains and tears.
A muscle strain is a common injury to a muscle or tendon that occurs when a muscle is stretched excessively. The most common type of strain injuries is hamstring strains, followed by gastrocnemius and soleus strains, quadriceps strains, lumbar strains, and thigh adductor strains. Complete muscle tears are seen less frequently.
Most athletes can return to their sports activities after appropriate diagnosis and treatment of muscle strain injuries. Prevention of reinjury is the major goal after treatment because reinjury is common; hamstring reinjury rates range from 12% to 31%.1 In this article, we discuss the anatomy and pathophysiology of strain injury, the biology of the muscle healing process, the clinical diagnosis of strains and tears, and various treatment and prevention strategies.
Anatomy and pathophysiology
Muscle groups are composed of tendon-muscle-tendon units that span one or more joints. Contractions of muscle groups induce and control joint motions. For example, the hamstring muscles (semimembranosus, semitendinosus, and biceps femoris) run from the pelvis and femur to the back and side of the knee; with their attached bones, they make up contractile units that stabilize the knee and hip and allow their motion (Figure 1). Injury occurs at the weakest part of the unit.
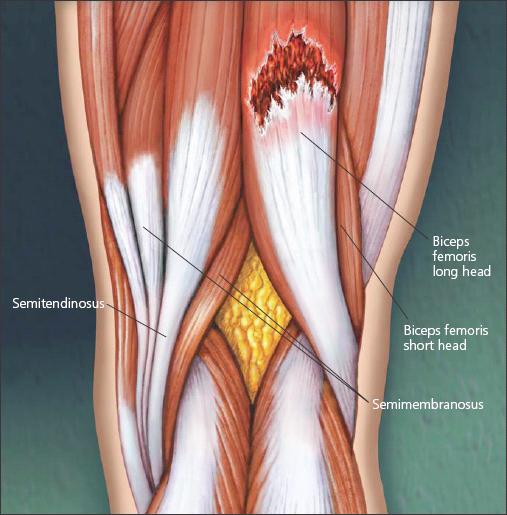
Figure 1 –
The most frequently strained muscle group is the hamstring,which consists of the semimembranosus, semitendinosus, and biceps femoris muscles.The hamstring is more susceptible to strain injury because it crosses more than 1 joint. A muscle tear of the long head of the biceps femoris is illustrated.
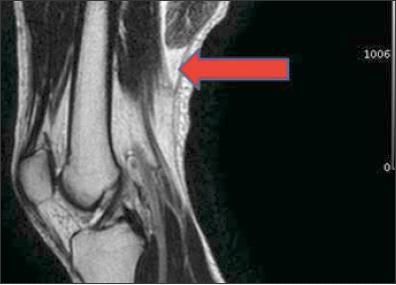
Figure 2 –
Shown here on a T2-weighted MRI scan is a complete tear of the distal end of the long head of the biceps femoris (arrow) with retraction.
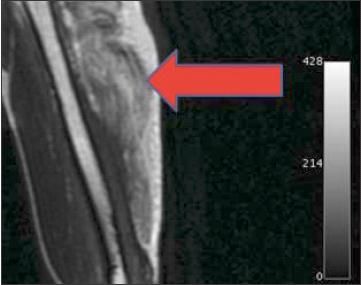
Figure 3 –
A severe strain of the long head of the triceps is demonstrated here by the increased signal intensity on the MRI scan (arrow).
At the microscopic level, skeletal muscle is composed of contractile and connective tissue elements. Actin and myosin myofilaments constitute the sarcomeric units of muscle fibers, which are surrounded by endomysium and arranged in bundles. Satellite cells surround the muscle fibers; these stem cells are important for tissue regeneration after injury. Muscle bundles are surrounded by perimysium and then by epimysium. Greater degrees of muscle injury tend to involve larger amounts of connective tissue disruption.
Muscle stretch is resisted by interaction between the contractile units and the surrounding connective tissues. As stretch moves beyond the physiological range, resistance shifts progressively from the contractile elements to the connective tissues.
The most common site of strain injury is the myotendinous junction, a region of highly folded basement membranes between the end of the muscle fiber and the tendon. These involutions maximize surface area for force transmission. However, the transition from compliant muscle fibers to relatively noncompliant tendon probably accounts for the unique vulnerability of the myotendinous junction.
Of note, the myotendinous junction usually spans a large surface area of the muscle belly (as opposed to the sharp demarcation often depicted in schematic diagrams). For example, the proximal and distal myotendinous junctions of the hamstrings actually overlap on the posterior and anterior surfaces of the muscle. This anatomical detail explains why, on clinical evaluation, strain injuries occurring at the myotendinous junction produce swelling, ecchymosis, and tenderness over a surprisingly large surface area.
Muscle contractions are categorized according to the sarcomeric length changes that occur during muscle activation. Isometric contractions involve muscle tension but no muscle shortening or lengthening. Concentric contractions involve muscle shortening; tension tends to be proportional to the force induced by the contractile elements. Eccentric contractions occur during muscle lengthening (resistance to stretch). The magnitude of contractile effort and the velocity of lengthening affect eccentric contractions; the resultant forces are large.
Most muscle strains and tears occur during eccentric contraction. Muscles that cross 2 joints (eg, hamstrings, gastrocnemius) are particularly vulnerable to stretch injury, because these muscles are affected by the simultaneous angular positions and angular velocities of adjacent joints.
Fiber type and, thereby, muscle fiber composition also affect susceptibility to muscle strain injury. Type I fibers generally are slow-twitch, oxidative fibers that have low glycogen levels and large numbers of mitochondria; they are fatigue-resistant. Type II fibers generally are faster-twitch and have variable oxidative dependencies. Type IIB fibers (fast, glycolytic) appear to be specifically vulnerable to muscle stretch injury.
Muscle activation alone usually is insufficient to cause significant strain injury in a healthy musculotendinous unit. Disruption at the myotendinous junction typically requires stretch beyond a threshold length of the entire musculotendinous unit.This pathogenic stretch can be passive or active; however, multiple animal studies have demonstrated that overt tissue failure tends to be length-dependent.2 The major difference between active and passive stretch injury is the larger energy force absorbed by the muscle group during active stretch before tissue failure.
A consistent sequence of events occurs after muscle fiber injury.3 The first phase involves acute inflammation, which is maximal in the first 24 to 48 hours after injury. The next phase involves removal of detritus, satellite cell activation, and subsequent fiber regeneration; this phase can last as long as 6 to 8 weeks after injury. The final phase involves tissue remodeling. It is important to recognize that complete tissue recovery involves delicate and finely coordinated elements of cellular and metabolic inflammatory reactions.
Clinical evaluation of muscle injury
Specific physical features may contribute to muscle strains and tears, such as bone structure, muscle-tendon imbalance, and growth spurts. Other causes include training errors and poor biomechanics. These injuries generally occur at 2 distinct times: at the beginning of an exercise program because of deconditioning and at the peak of training when the athlete is striving for improvement.
Most patients present with muscle strain injuries after an acute onset of pain during activity. A thorough history is needed to distinguish among acute, chronic, and "acute on chronic" injuries. The mechanism of injury may help predict the diagnosis. Always inquire about previous muscle strains or prodromal muscle soreness, which may influence both treatment and avoidance strategies.
Physical examination may reveal localized swelling, ecchymosis, or both. This may evolve over the course of several days. Palpation usually reveals tenderness over the myotendinous junction. A palpable defect may indicate a significant partial tear or a complete rupture. Active and passive range of motion usually is painful and limited.
Always include a neurovascular examination and a comparative evaluation of the opposite extremity. Compartment syndrome (a surgical emergency) is quite rare in this setting, but it can occur. Hallmark features include swelling, pain with passive stretch, and increased intramuscular pressure.
The differential diagnosis of muscle strains is broad. It should include tendon tears, tendinitis, stress fracture, muscle contusion, hematoma, avulsion fracture and, rarely, intramuscular infection.
Imaging techniques
Radiographs should be obtained initially, especially in adolescent athletes. They may demonstrate only soft tissue swelling, but they also may reveal more. Fracture, avulsion fracture, and severe underlying pathology can be ruled out with simple radiographs.
Ultrasonography is becoming a first-line technique in detecting superficial muscle strains and tears, especially proximal myotendinous junction tears. Distal myotendinous junction tendon tears rarely require ultrasonography for diagnosis. Diagnosis of these strains/tears is based on a good history and physical examination.
The ultrasonographic appearance of a muscle strain or tear ranges from an ill-defined hyperechoic area in less severe injuries to a hypoechoic area surrounded by a hyperechoic halo resulting from blood infiltration of the surrounding muscle.4 Ultrasonography also may be used for guidance of hematoma drainage in acute injuries.
The benefits of ultrasonography include easy accessibility and low cost, and it is noninvasive. It can confirm a clinical diagnosis, assess the extent of damage, and reveal a tear not suspected clinically.4 Ultrasonography also can be used to verify healing, which allows patients earlier return to sports activity. Disadvantages include a lack of operator experience, a slow learning curve, and potentially limited reimbursement because of the newer application of this technology.
MRI may be a more sensitive measure because of sonographer experience. It may be helpful if the diagnosis is unclear, if physical examination findings are out of proportion to the mechanism of injury or objective findings, or if it is important to quantify injury severity in a high-level athlete (Figures 2 and 3). Hematoma and interstitial edema are well visualized on T2- weighted images. MRI also may be helpful in the evaluation of complete tears with tendon retraction for surgical decision making.
Classification schemes are described for muscle strain injuries, but injury classification usually does little to change treatment decisions.5 From a practical perspective, injuries may be described as mild, moderate, or severe (complete tear). This assessment is based on the amount of fiber injury, which may be estimated from the degree of swelling, pain, and fiber discontinuity. MRI is somewhat useful in this regard.The greatest value of injury classification is estimation of the anticipated time to return to sports activity. Disadvantages of MRI are lack of accessibility, prolonged examination time, and high cost.
Treatment
The mnemonic RICE is still the mainstay of acute management of muscle strain injuries; rest, ice, compression, and elevation all help decrease swelling and pain. Control and resolution of swelling and recovery of range of motion are the 2 major goals. An appropriate rest interval should allow for healing and recovery of muscle function, which has been shown to decrease sharply in the first few days after acute strain injury in animal models.6
Cryotherapy is an important part of initial treatment, although the basic science of cold therapy is not well delineated. Cryotherapy is thought to work by decreasing local blood flow by means of vasoconstriction, thereby decreasing edema formation. Cold treatment probably also disrupts the pain cycle through counterstimulation or modulation of pain impulse transmission. Regardless, cryotherapy is inexpensive, readily available, easy to apply, and relatively safe.
NSAIDs, another mainstay of muscle strain treatment, work to block prostaglandin formation and decrease pain associated with the inflammatory response. Although they are used commonly, some controversy exists over their long-term use. Mishra and associates7 evaluated rabbit muscle function after exercise-induced injury with 6 days of flurbiprofen or placebo administration. Contractile, histological, and structural analyses demonstrated greater functional recovery at 3 and 7 days in the NSAID-treated group but decreased force production at 28 days after injury. Short-term benefit also was noted by Obremsky and coworkers8 up to 7 days after strain injury with piroxicam treatment in rabbits.
The cyclooxygenase (COX) enzymes have been shown to play a role in satellite cell proliferation, fusion, and differentiation; COX-2 inhibition has been linked to a decreased satellite cell proliferation in rats.9 Recall that satellite cell activation is necessary for repair of a muscle strain. A recent study conducted by Mackey and associates10 on the effects of treatment with indomethacin, a nonselective COX inhibitor, in endurance runners showed inhibition of satellite cell proliferation after a 36-km run. Selective COX-2 inhibitor human studies have yet to be performed, but there is evidence that these agents may be counterproductive in repair of muscle injury because COX-2 plays a role in satellite cell proliferation.
Although it is likely that early NSAID treatment may be beneficial for decreasing the acute pain and inflammation after muscle strain, prolonged treatment (weeks to months) may have some mild adverse effect on muscle recovery.11 These medications have major value in facilitating rehabilitation through their analgesic qualities, but analgesia also may be achieved with other types of medications.
Prolonged immobilization after strain injury should be avoided because of the potential for permanent stiffness. However, a short period of immobilization after severe strain injury may be reasonable for pain relief and for protection during the initial phases of the healing response. In a study of rat gastrocnemius injury, Jrvinen and Lehto12 noted some improvement in the orientation of muscle fiber regeneration with less scar formation after a short period of immobilization followed by mobilization.
An exercise program should be instituted as soon as the patient's pain and swelling subside to progressively recover range of motion, strength, endurance and, ultimately, normal athletic skills. Supervision of this program by a physical therapist or athletic trainer is reasonable after significant muscle strain injury. Some physicians suggest return to sports activity when there is 80% return of strength compared with the noninjured side.
Surgery may be indicated in the rare instance of a complete tear with significant retraction of the muscle from the tendon. However, repair is quite difficult; muscle fibers do not hold sutures reliably.
Prevention
Recurrence of injury is very common without appropriate rehabilitation; return to activity before full recovery in sports such as running and tennis often results in recurrence. Steps should be taken to prevent recurrence, as well as identify those at risk for a first-time muscle strain injury.
Strength imbalance is thought to be one of the factors contributing to muscle strain injury. In a study comparing muscle strain injuries in professional soccer players with strength imbalance with those without imbalance, the risk of injury was significantly higher in players with the imbalance.13 Preseason screening for strength imbalance may be a valuable tool; intervention would be indicated for the players found to have a strength imbalance.
In addition to strength imbalance, muscle atrophy is another factor to consider in older persons who are living more active lifestyles and participating in sports activities. A study conducted by Kubo and colleagues14 found that older persons have lesser force generation capabilities and tendon extensibilities of knee extensors and plantar flexors. These weaknesses in strength and flexibility should be addressed to help prevent strain injuries.
A study on the effects of a 6-week intervention program involving in vivo lengthening contractions in young and old rats was performed, comparing differences in force deficit and muscle fiber breakage rates.15 After the 6-week program, no differences were found between the young and old rats.This result shows that some of the age-related weaknesses that contribute to muscle strains may be able to be managed with intervention.
Although controversial, stretching before physical activity can help prevent muscle strain injury. Hartig and Henderson16 studied effects of a stretching program in military basic training.The control company proceeded through normal basic training; the intervention company added 3 hamstring stretching sessions to the program. In the intervention group, hamstring flexibility increased and the frequency of injuries was significantly lower than in the control group (16.7% vs 29.1%).
Appropriate warm-up activity also should be a part of strain injury prevention, because warm muscles are more flexible and failure- resistant.17 In summary, flexible, strong, and warmed-up muscles are the goals of strain injury rehabilitation, as well as injury prevention.18,19
References:
References
1.
Petersen J, Hölmich P. Evidence based prevention of hamstring injuries in sport.
Br J Sports Med.
2005;39:319-323.
2.
Garrett WE Jr. Muscle strain injuries.
Am J Sports Med.
1996;24(suppl 6):S2-S8.
3.
Leadbetter WB. Soft tissue athletic injury. In: Fu FH, Stone DA, eds.
Sports Injuries: Mechanisms, Prevention, Treatment.
2nd ed. Philadelphia: Lippincott, Williams & Wilkins; 2001:839-888.
4.
Bianchi S, Poletti PA, Martinoli C, Abdelwahab IF. Ultrasound appearance of tendon tears, part 2: lower extremity and myotendinous tears.
Skeletal Radiol.
2006;35:63-77.
5.
Ryan AJ. Quadriceps strain, rupture, and charlie horse.
Med Sci Sports.
1969;1:106-111.
6.
Nikolaou PK, Macdonald BL, Glisson RR, et al. Biomechanical and histological evaluation of muscle after controlled strain injury.
Am J Sports Med.
1987;15:9-14.
7.
Mishra DK, Fridén J, Schmitz MC, Lieber RL. Antiinflammatory medication after muscle injury: a treatment resulting in short-term improvement but subsequent loss of muscle function.
J Bone Joint Surg.
1995; 77A:1510-1519.
8.
Obremsky WT, Seaber AV, Ribbeck BM, Garrett WE Jr. Biomechanical and histologic assessment of controlled muscle strain injury treated with piroxicam.
Am J Sports Med.
1994;22:558-561.
9.
Mendias CL, Tatsumi R, Allen RE. Role of cyclooxygenase-1 and -2 in satellite cell proliferation, differentiation, and fusion.
Muscle Nerve.
2004;30:497-500.
10.
Mackey AL, Kjaer M, Dandanell S, et al. The influence of anti-inflammatory medication on exerciseinduced myogenic precursor cell responses in humans.
J Appl Physiol.
2007;103:425-431.
11.
Almekinders LC. Anti-inflammatory treatment of muscular injuries in sport: an update of recent studies.
Sports Med.
1999;28:383-388.
12.
Järvinen MJ, Lehto MU. The effects of early mobilisation and immobilisation on the healing process following muscle injuries.
Sports Med.
1993;15:78-89.
13.
Croisier JL, Ganteaume S, Binet J, et al. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study.
Am J Sports Med.
2008;36:1469-1475.
14.
Kubo K, Ishida Y, Komuro T, et al. Age-related differences in the force generation capabilities and tendon extensibilities of knee extensors and plantar flexors in men.
J Gerontol A Biol Sci Med Sci.
2007;62:1252-1258.
15.
Lynch GS, Faulkner JA, Brooks SV. Force deficits and breakage rates after single lengthening contractions of single fast fibers from unconditioned and conditioned muscles of young and old rats.
Am J Physiol Cell Physiol.
2008;295:C249-C256.
16.
Hartig DE, Henderson JM. Increasing hamstring flexibility decreases lower extremity overuse injuries in military basic trainees.
Am J Sports Med.
1999;27:173-176.
17.
Noonan TJ, Best TM, Seaber AV, Garrett WE Jr. Identification of a threshold for skeletal muscle injury.
Am J Sports Med.
1994;22:257-261.
18.
Noonan TJ, Garrett WE Jr. Muscle strain injury: diagnosis and treatment.
J Am Acad Orthop Surg.
1999;7:262-269.
19.
Brothers A, Alamin T, Pedowitz R. Basic clinical management of muscle strains and tears.
J Musculoskel Med.
2003;20:303-307.