Article
Common Isolation Units Demonstrate Mixed Outcomes for Clostridium Difficile Patients
Author(s):
Data showed that 30-day mortality rates were significantly lower in CIU patients (18.8%) in comparison to original bed patients (34%).
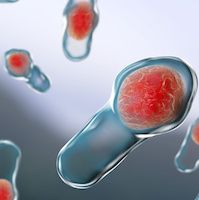
In order to evaluate the effectiveness of isolating patients with Clostridium difficile infection (CDI) as strategy to reduce spread of CDI and improve outcomes for patients, Dante Alí García-Lecona, MD, with the José Eleuterio González University Hospital in Monterrey, Mexico, led a 3-year long study in which CDI patients were treated in a common isolation unit (CIU) rather than in general hospital beds.
The study, which created a 1-room, 4-bed CIU for CDI diagnosed patients, discovered that patients treated in the CIU unit as opposed to their bed of diagnosis saw decreases in mortality rates and antibiotic use, but higher recurrence rates for CDI.
The study took place at the José Eleuterio González University Hospital, a 500-bed hospital with common rooms that have 2-8 beds and a small proportion of individual rooms (<10%). The CIU established by the study was isolated from general population, and housed up to 4 CDI patients at a time. One to 2 nurses and a single medical attendant were devoted to the unit.
García-Lecona and colleagues reported that all CDI diagnosed patients were transferred to the CIU during the 3-year study period except those patients in critical care, the surgical ward, or if the CIU was full. During the January 2014—December 2016 study period, García-Lecona reported 176 total patients were diagnosed with CDI; 48.2% of those patients (n=85) were isolated in the CIU, and the remaining 51.7% (n=91) remained in their original bed.
Resulting data from the study showed there were statistically significant differences between the CIU and original bed patients in terms of mortality rates, antibiotic use, and recurrence rates. Data from the study showed that 30-day mortality rates were significantly lower in CIU patients (18.8%) in comparison to original bed patients (34%).
Patients in the CIU also reportedly received an average of 1 day less antibiotic treatment (average 8.2 days) than patients in the original bed group (average 9.2 days). Patients in the CIU did receive higher numbers of fecal microbiota transplant (FMT) at a rate of 23.52% (n = 20) versus patients in original beds, where only 4.3% of patients (n=4) received FMT.
There was a higher incidence of recurrence of CDI in CIU patients versus original beds patients (14 versus 7, respectively; P= .081), but García-Lecona and colleagues report that the difference in recurrence was not statistically significant. No detectable data suggested that the use of CIU for CDI patients affected the overall CDI rates in the hospital as a whole.
García-Lecona and colleagues write that "management of CDI patients in healthcare settings poses a complex balance between clinical treatment and prevention of spreading." They believe the creation of isolation units for patients with diagnosed CDI could offer some safeguards against the spread of hospital-acquired CDI and serve as a means of hospital infection control. An additional advantage that may help lower mortality rates among patients in the CIU is to lower nurse to patient ratio, which García-Lecona writes "might have positively influence mortality and lowered treatment duration."
The researchers caution, however, that grouping CDI patients in CIU did result in an increased rate of re-infection which "despite standard environmental disinfection techniques, is probably caused by the persistence of spores in the environment."
While the researchers believe that the use of a CIU dedicated to the management of CDI patients could provide a clinical advantage for some hospitals and may be a useful component of "a multifaceted intervention," the use of CIU did not demonstrate a reduction in CDI spread.
The use of CIU, García-Lecona reports, has been evaluated during CDI outbreak scenarios to some effect, but the isolation of CDI infected patients provided mixed results during their non-epidemic study scenario — while it did improve CDI patient outcomes, it did not lower the rates of CDI among the patients as a whole.
"Outcomes of Clostridium difficile—infected patients managed in a common isolation unit compared with isolation in their bed of diagnosis" appears in the January 2018 issue of American Journal of Infection Control.
Related Coverage >>>
Future of FMT May Depend on New AGA Registry
The Best Defense Against Hospital-Acquired Infections
Effectiveness of Fidaxomicin Versus Vancomycin for Clostridium Difficile Treatment





