A Diagnosis for the Doctor's Digits?
A 50 year-old physician experienced the abrupt onset of tenderness and swelling in the distal interphalangeal (DIP) joint of his right index finger. His only significant past medical history was Wolf-Parkinson-White syndrome, which was managed successfully with ablation. The same symptoms subsequently occurred in the DIP joints of his left index finger and fifth digits of both hands. No other digits were affected. The symptoms made it difficult for him to type on the computer. He denied trauma to the affected fingers, although he is an athlete and had had a left middle finger avulsion fracture, right middle finger dislocation, and left radial frac-ture. He had no systemic or other joint involvement.
A 50 year-old physician experienced the abrupt onset of tenderness and swelling in the distal interphalangeal (DIP) joint of his right index finger. His only significant past medical history was Wolf-Parkinson-White syndrome, which was managed successfully with ablation. The same symptoms subsequently occurred in the DIP joints of his left index finger and fifth digits of both hands. No other digits were affected. The symptoms made it difficult for him to type on the computer. He denied trauma to the affected fingers, although he is an athlete and had had a left middle finger avulsion fracture, right middle finger dislocation, and left radial frac-ture. He had no systemic or other joint involvement.
There was no family history of connective tissue disease, psoriasis, or other arthritis conditions. The patient had no allergies, took no medication, and did not smoke cigarettes or abuse alcohol or drugs.
On examination, there was swelling and tenderness of the DIP joints of the patient's index and fifth digits bilaterally. The DIP joints of both index fingers and of the right fifth digit were laterally subluxed. There was no erythema or metacarpophalangeal (MCP) or proximal interphalangeal (PIP) joint involvement, and the hand and wrist examination results were otherwise normal, as were the rest of the physical examination results. Also normal were the complete blood cell (CBC) count, 20-item chemistry panel, rheumatoid factor (RF), anticyclic citrullinated peptide (anti-CCP) antibody, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) level.
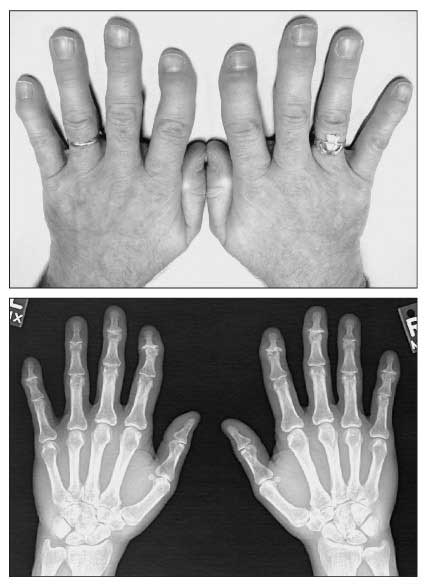
A clinical photograph (top) and x-ray film (bottom) of both hands are shown.
What is your diagnosis?
(Find the answer on the next page.)
This patient had erosive osteoarthritis (OA), an unusual entity that most often involves the PIP and DIP joints of the hand. Erosive OA differs from typical nonerosive interphalangeal joint OA in that bony erosions develop in affected joints.
The onset of erosive OA typically is abrupt, and the course may be rapidly progressive. The DIP joints usually are affected first. Involved joints become stiff, swollen, tender, and erythematous; over time, deformities (eg, subluxations) may develop. The inflammatory episodes occur intermittently; joint involvement ultimately becomes symmetrical. Any digit may be affected, but the MCP and carpal joints and other joints of the body usually are spared. There is no systemic involvement.
Erosive OA occurs more frequently in women than in men.1 The average age at disease onset is 50 years.
The causes of erosive OA are poorly understood. Recent evidence indicates a genetic predisposition, as shown by an increase in HLA-DRB1 antigens in persons with erosive OA versus those with nonerosive OA.1The complete metabolic profile and CBC count, RF, and anti-CCP antibody results are normal in patients with erosive OA.1-3 The ESR and CRP level may be mildly elevated. Radiographs of the hands show joint-space narrowing, gull-wing deformities and, sometimes, subluxations; these changes are similar to those seen in nonerosive OA. In erosive OA, however, affected joints also show central erosions and severely involved joints may become ankylosed. Bone density is preserved.1,2
The differential diagnosis includes rheumatoid arthritis (RA) and psoriatic arthritis (PsA).1,2 Like erosive OA, RA causes erosive changes in the finger joints. However, RA differs from erosive OA in several ways. In RA, the MCP joints are affected and the DIP joints are spared. RA is a systemic rather than localized disease. RF and anti-CCP antibodies often are present, and the ESR and CRP level may be markedly elevated. In RA, radiographs show periarticular osteopenia but no ankylosis and marginal rather than central erosions.
PsA, like erosive OA, involves the DIP joints, and severe involvement may lead to joint ankylosis. In both PsA and erosive OA, bone density usually is preserved. However, patients with PsA have psoriatic skin changes, often with fingernail abnormalities, and axial and other joints are affected.
Very little information is available about treatment for patients with erosive OA. Hydroxychloroquine (HCQ) has been reported to decrease pain and swelling,4 and we have used it successfully in other patients with erosive OA. Chondroitin sulfate also may alleviate symptoms and, possibly, retard further joint damage.1 Our patient was given a prescription for HCQ but had not started it at the time of his follow-up visit.
References:
1.
Punzi L, Ramonda R, Sfriso P. Erosive osteoarthritis.
Best Pract Res Clin Rheumatol
. 2004;18:739-758.
2.
Belhorn LR, Hess EV. Erosive osteoarthritis.
Semin Arthritis Rheum
. 1993;22:298-306.
3.
Morozzi G, Bellisai F, Fioravanti A, Galeazzi M. Absence of anti-cyclic citrullinated peptide antibodies in erosive osteoarthritis: further serological evidence of the disease as a subset of osteoarthritis.
Ann Rheum Dis
. 2005;64:1095-1096.
4.
Bryant LR, des Rosier KF, Carpenter MT. Hydroxychloroquine in the treatment of erosive osteoarthritis.
J Rheumatol
. 1995;22:1527-1531.
This case was submitted by Kiran Qidwai, a third-year medical student at the University of Illinois at Chicago College of Medicine, and Aakash Desai, MD, an internal medicine resident, and Catherine Meyer, MD, chief of rheumatology, at Mercy Hospital and Medical Center in Chicago.