Foot Pain After Parkour in a 31-Year-Old Man
A 31-year-old Asian man presented for evaluation of left foot pain that began on the day before his clinic visit while he was practicing parkour (the physical discipline of training to overcome obstacles within one’s path by using only the human body and objects in the environment). He had no significant medical history. The patient recalled leaping from a platform toward a horizontal bar attached to a wall a few feet away. During the lift-off phase of the jump, he experienced a snapping sensation in his left foot, with subsequent pain in the arch and heel. Immediately after this event, he was unable to ambulate.
A 31-year-old Asian man presented for evaluation of left foot pain that began on the day before his clinic visit while he was practicing parkour (the physical discipline of training to overcome obstacles within one’s path by using only the human body and objects in the environment). He had no significant medical history. The patient recalled leaping from a platform toward a horizontal bar attached to a wall a few feet away. During the lift-off phase of the jump, he experienced a snapping sensation in his left foot, with subsequent pain in the arch and heel. Immediately after this event, he was unable to ambulate.

The patient denied any recent trauma or any use of corticosteroids or fluoroquinolones in his lifetime. He did have a long-term history of intermittent and alternating aches on the heels of his feet. However, he had experienced pain in only his right (opposite) foot in the weeks before this acute injury.
The patient arrived at our office on crutches with an elastic bandage wrapped around his left midfoot and ankle. Visual inspection revealed minimal ecchymosis and mild swelling along his left heel and arch. He demonstrated an antalgic gait, with worsened pain on resisted dorsiflexion of the left foot.
The patient was neurovascularly intact, with normal strength of both feet and ankles. No palpable masses were appreciated. The Achilles
tendon was intact and nontender, with a normal Thompson squeeze test result (while the patient lies prone with both feet extending past the end of the table, the clinician squeezes the calf of the affected leg; plantar flexion suggests normal Achilles tendon response, and a lack indicates Achilles tendon rupture). Findings from the remainder of the examination of both feet and ankles were unremarkable.
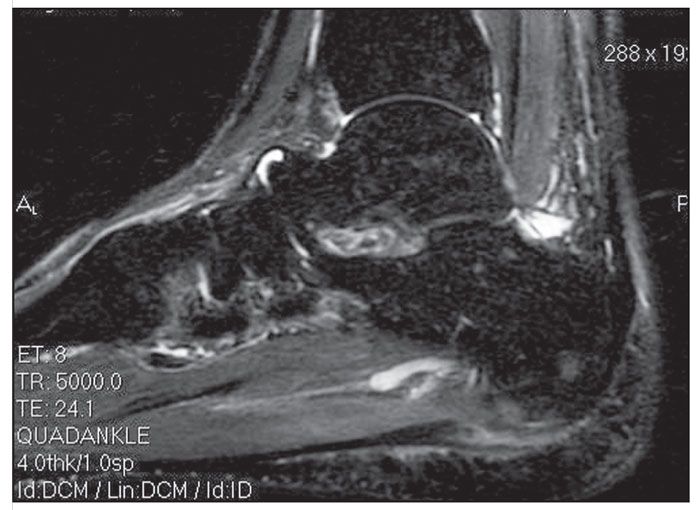
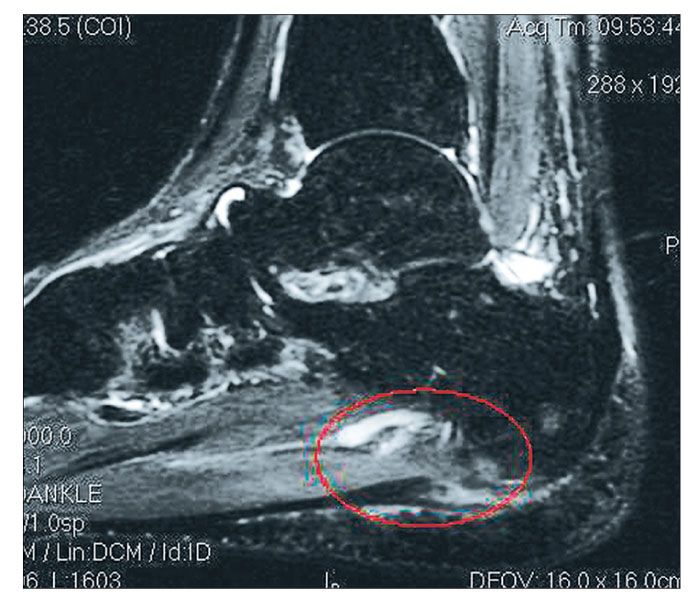
A lateral x-ray film of the patient’s left foot (above, left) and a sagittal MRI scan with short tau inversion recovery (STIR) sequences (below, left) were obtained and are shown.
What is your diagnosis?
(Find the answer on the next page.)
The diagnosis was a partial plantar fascia rupture. Key components of the history and physical examination may suggest such a diagnosis.
Most patients with a partial or complete rupture of the plantar fascia present with a history of a tearing or snapping sensation on the plantar aspect of their foot after intense acceleration activities, such as running and jumping.1 The patient usually cannot continue regular activity or walk because of pain.2 In addition, there may be swelling and development of ecchymosis, possibly with a tender lump, on the medial aspect of the heel.3 This ecchymosis, when present, develops 1 to 4 days after the injury.2
A noted association between plantar fascia ruptures and previous plantar fasciitis symptoms or corticosteroid injections has been documented in the literature.1,2,4-6 Although our patient denied a history of corticosteroid injections, he did note a history of heel pain that alternated between his feet, suggestive of plantar fasciitis.
The x-ray films were nondescriptive and demonstrated no calcaneal spurs or other bony abnormalities. However, the MRI STIR sequences showed an abnormality of the medial aspect of the plantar fascia (ellipse), with thickening of the fascia distal to this region, and soft tissue edema in the adjacent area, confirming the diagnosis of a partial plantar fascia rupture.
MRI characteristics for the diagnosis of plantar fascia rupture include (1) complete or partial interruption of the low-signal-intensity plantar fascia with high T2/STIR signal (probably representing hemorrhage, inflammation, and edema) and (2) associated injuries of the underlying flexor digitorum brevis muscle demonstrated by the presence of high T1 and T2 signal representing hemorrhage and edema.7 If MRI is not feasible, an alternative would be ultrasonography, which may demonstrate (1) disruption of the plantar fascia and (2) hypoechoic tissue in the region of rupture resulting from inflammation and hemorrhage.7
In addition to plantar fasciitis, the differential diagnosis includes plantar fibromatosis, plantar xanthomas, calcaneal spurs with heel pad atrophy, calcaneal stress fractures, tarsal tunnel syndrome, medial calcaneal nerve neuroma, malignancy, and osteomyelitis. The acuity of the patient’s symptoms in conjunction with the imaging studies helped confirm our diagnosis.
Although the literature pertaining to plantar fascia rupture is limited, Saxena and Fullem8 formulated a conservative treatment protocol for the patient population with this injury.1 Our patient underwent symptomatic treatment with rest, ice, and elevation, as well as naproxen, 500 mg twice a day, taken orally for 10 days. In addition, he was placed in a short-leg walking boot, and with the use of crutches, he was strictly non–weight bearing for 3 weeks. In the interim, he was referred to podiatry; an additional recommendation was made for a compression stocking to reduce swelling.
By about 3 weeks postinjury, the patient began weight bearing as tolerated and was referred to physical therapy for stretching, strengthening, and proprioception exercises. By 10 weeks postinjury, he was performing low-impact activities; by 16 weeks, he reported no pain with intense acceleration activities.
References:
1. Leach R, Jones R, Silva T. Rupture of the plantar fascia in athletes. J Bone Joint Surg. 1978;60A:537-539.
2. Ahstrom JP Jr. Spontaneous rupture of the plantar fascia. Am J Sports Med. 1988;16:306-307.
3. Rolf C, Guntner P, Ericsäter J, Turan I. Plantar fascia rupture: diagnosis and treatment. J Foot Ankle Surg. 1997;36:112-114.
4. Sellman JR. Plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1994;15:376-381.
5. Acevedo JI, Beskin JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1998;19:91-97.
6. Herrick RT, Herrick S. Rupture of the plantar fascia in a middle-aged tennis player: a case report. Am J Sports Med. 1983;11:95.
7. Jeswani T, Morlese J, McNally EG. Getting to the heel of the problem: plantar fascia lesions. Clin Radiol. 2009;64:931-939.
8. Saxena A, Fullem B. Plantar fascia ruptures in athletes. Am J Sports Med. 2004;32:662-665.