Hydralazine: A Drug Whose Time has Come and Gone?
Hydralazine has one--and only one--robust evidence-based indication, this author says. So why is it still prescribed beyond that?
©molekuul_be/Shutterstock.com
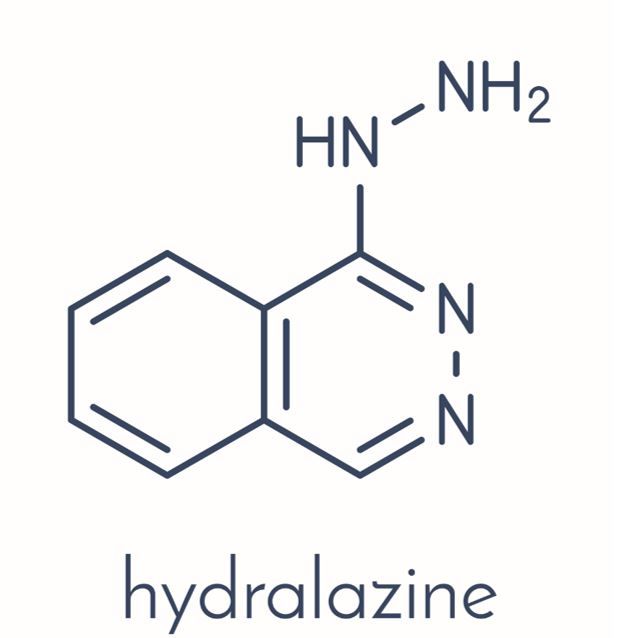
In the last few weeks, I have seen multiple patients taking hydralazine. As best I can tell, hydralazine has one-and only one-“robust,” evidence-based indication: the treatment of systolic heart failure in African-American patients.
The majority of patients that I saw did not have an evidence-based indication. They either had hypertension, were experiencing diastolic dysfunction, and/or avoiding an ACEI or an ARB for some reason (usually side effects). As I have wondered in the past about the use of beta-blockers for cardiac patients with hypertension, I must ask why hydralazine has persisted as a therapeutic agent contrary to the best evidence.
First, in regard to essential hypertension, there are no randomized, placebo controlled trials of hydralazine for this indication.1 The conclusion of a Cochrane Database System Review a few years back was, “hydralazine may reduce blood pressure when compared to placebo in patients with primary hypertension, however these data are based on before and after studies, not RCTS. Furthermore, its effect on clinical outcomes remains uncertain.”1 In an era where antihypertensive agents not only lower blood pressure, but also add other substantial benefits (cardioprotection, reduced proteinuria) hydralazine is not good enough for primetime.
Next, the list of hydralazine side effects should also give one pause. Peripheral neuropathy, blood dyscrasias, SLE complicated by glomerulonephritis, purpura, and hepatitis can occur.2 If hydralazine is administered without a beta blocker, the compensatory tachycardia is unwelcome in patients with coronary disease. At least one half of the recent patients I encountered on hydralazine were not on beta blockade.
Unlike ACEIs and ARBS, hydralazine dilates the afferent glomerular arteriole, increasing intraglomerular pressure.3 This glomerular hyperfiltration is exactly what is unwanted in patients with diabetes and albuminuria.
Finally, the frequency of hydralazine’s dosing schedule makes compliance difficult.
So, it is time to ask: why is “eminence-based” medicine (not evidence-based) resuscitating hydralazine?
Have some thoughts on the matter? Please send them to editor@patientcareonline.com
References:
1. Kandler MR, Mah GT, Tejani AM, Stabler SN, Salzwedel DM. Hydralazine for essential hypertension. Cochrane Database Syst. Rev. 2011; 11:CD004934.
2. McComb M, Chao JY, Ng TM. Direct vasodilators and sympatholytic agents. Cardiovasc Pharmacol Rev. 2016; 21:3-19.
3. Wolf S, Risler T. Are all antihypertensive drugs renoprotective? Herz 2004; 29:248-254.