Managing Plantar Fasciitis and Other Heel Pain
Heel pain (calcaneodynia) is most commonly due to plantar fasciitis, but has many other causes including nerve entrapment, stress fracture, and sciatica. This review describes an overall approach to diagnosis, discusses conservative treatments and highlights the most prevalent surgical procedures.
Heel pain (calcaneodynia) is the most frequent complaint of patients evaluated by foot and ankle specialists. The most common cause is plantar fasciitis, an inflammation of the origin of the plantar fascia. This results from a biomechanical imbalance that produces excessive tension along the plantar fascia. Heel pain may also have a neurological, traumatic, or systemic origin.
Other conditions (eg, tibia vara, ankle equinus, and hindfoot or forefoot varus) can cause increased pronation with strain of the longitudinal arch. This results in additional stress on the anatomical medial band of the plantar fascia and may lead to plantar fasciitis.1,2
Although heel pain is common, much confusion remains about the causes, prognosis, and management of its underlying conditions. In this article, we describe an overall approach to the diagnosis of plantar fasciitis and other causes of heel pain. We also discuss various conservative treatment options and highlight the most frequently used surgical procedures.
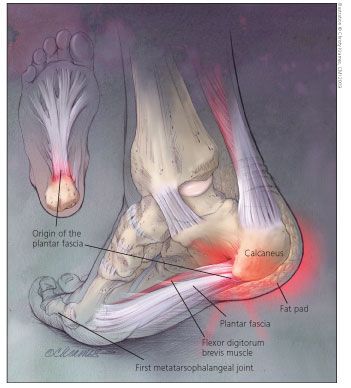
Figure – The plantar fascia is a broad ligament that originates along the inferior aspect of the calcaneus, spans the plantar aspect of the foot, and inserts into the plantar plates of the metatarsophalangeal joints and the proximal portions of the toes. The origin of the plantar fascia at the medial tubercle of the calcaneus is the most common site of pain (inset). Typically, inferior calcaneal spurs are found at the origin of the flexor digitorum brevis muscle dorsal to the plantar fascia. Inflammation of the plantar fascia, rather than heel spurs, is the source of pain.
DIAGNOSISAnatomy
The plantar fascia is a broad ligament just dorsal to the foot's subcutaneous fatty tissue (Figure). It originates along the inferior aspect of the calcaneus, spans the plantar aspect of the foot, and inserts into the plantar plates of the metatarsophalangeal (MTP) joints and the proximal portions of the toes. In dissection of 200 cadaveric specimens, Barrett and associates3 found 3 bands proximally: medial, central, and lateral. The plantar fascia was between 2 and 4 mm in thickness; the medial band averaged 4.4 mm, roughly twice as thick as the lateral and central bands.
Dorsal to the plantar fascia lies the origin of the flexor digitorum brevis (FDB) muscle, where typically, inferior calcaneal spurs are found. Medial to the FDB muscle is the abductor hallucis (AH) muscle, which has both deep and superficial fascia. The quadratus plantae (QP) muscle lies dorsal to the FDB.
The medial calcaneal nerve arises from the tibial nerve around the level of the medial malleolus and supplies sensation to the plantar medial aspect of the heel. The first branch of the lateral plantar nerve is a mixed nerve that provides innervation to the abductor digiti quinti (ADQ) muscle and the FDB. Because this nerve lies dorsal to the AH muscle, compression of it can cause heel pain.
The medial and lateral plantar nerves are situated between the FDB and QP muscles and provide sensation to the medial plantar and lateral plantar aspects of the foot, respectively. The sural nerve innervates the lateral aspect of the skin of the heel.
Causes
Plantar fasciitis occurs in both men and women but more frequently in men. Repetitive trauma results in microtears in the plantar fascia. Microtearing, and the body's attempted repair of it, results in chronic inflammation. Usually, the condition is caused by a change or increase in physical activities; wearing shoes that lack arch support, have little cushion, or do not easily bend under the ball of the foot; an acute injury; or prolonged standing. Often, the precise source of plantar fasciitis in a given patient is unknown.
Overweight is a common cause. The plantar fascia not only encapsulates muscles in the bottom of the foot but also supports the arch by acting as a bowstring that connects the ball to the heel.
During walking, at the moment when the heel of the trailing leg begins to lift off the ground, the plantar fascia endures tension that is about 2 times body weight. If the calf muscles lack flexibility, this moment of maximum tension is "sharpened" (increased suddenly). A percentage increase in body weight causes the same percentage increase in tension in the fascia.
Heel pain may occur in patients who have various systemic inflammatory conditions, including rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, Reiter syndrome, gout, Behet syndrome, and systemic lupus erythematosus. Rarely, gonorrhea and tuberculosis have been implicated as causes of heel pain.
History
Heel pain with the first few steps in the morning and after a period of rest is the classic symptom of plantar fasciitis. The pain improves with activity but recurs after prolonged weight bearing, often at the end of the day. Usually, the pain is felt in the front and bottom of the heel, but as the definition of "plantar fasciitis" indicates, it can be felt in any portion of the bottom of the foot where the fascia is located. Often, patients report that the pain is predominantly in the heel but radiates to the arch. If heel pain is not present, the diagnosis of plantar fasciitis must be questioned.
It is important to determine whether the patient's symptoms are acute or chronic. The acute onset of symptoms may suggest a calcaneal stress fracture, although this injury also may be insidious in onset. A history of trauma could suggest an acute plantar fascia tear or rupture.
Careful history taking may suggest a reason for the onset of pain, which may include recent weight gain or unusual activity, such as starting a walking or exercise program or prolonged standing. Amis and associates4 found that 70% of patients who have plantar fasciitis are obese. Complaints of burning and tingling in the feet or heel or both suggest tarsal tunnel syndrome, compression of the Baxter nerve, peripheral neuropathy, or sciatica.
The physical examination
In the evaluation of patients with plantar heel pain, several conditions should be considered. These include calcaneal stress fracture, fat pad atrophy, distal plantar fasciitis, rupture of the plantar fascia, entrapment of the nerve to the ADQ muscle (Baxter nerve), tarsal tunnel syndrome, sciatica, bone and soft tissue tumors, calcaneal apophysitis (Sever disease), inflammatory arthropathies, and infection. (For more discussion, see the Box, "Considering other causes of heel pain.)
The physical examination is critical in the evaluation of inferior or plantar heel pain. With the patient sitting in front of the examiner, the tension of the Achilles tendon should be determined with the Silverskjold test. Careful assessment of arch height should be undertaken with the patient standing, both kneecaps pointing straight ahead, and then asking the patient to bend the knees, placing stress on the arch.
Tenderness or swelling or both directly over the plantar calcaneal tuberosity and proximal plantar fascia suggests proximal plantar fasciitis (heel pain syndrome). Tenderness over the distal and middle portions of the plantar fascia suggests the less common distal plantar fasciitis. If the entire heel is tender, consider a stress fracture, a bone tumor or, in children, Sever disease.
In older patients, pain under the fat pad suggests fat pad atrophy. Tenderness to medial and lateral calcaneal compression could indicate a stress fracture.
Radiating pain under the AH muscle is present with Baxter nerve entrapment; tenderness with a positive Tinel sign (percussion of a damaged nerve elicits pain along the course of the nerve) in the tarsal tunnel may indicate tibial nerve compression. A positive Lasgue sign (with the patient in a supine position and the hip flexed, knee extension elicits pain along the course of the sciatic nerve) should alert the physician to the possibility of sciatica (lumbar radiculopathy).
A firm nodule adherent to the plantar fascia suggests a plantar fibroma. Swelling, tenderness, and ecchymosis in the proximal arch occur with plantar fascia rupture. Localized tenderness, swelling, warmth, and erythema are signs of possible soft tissue infection or osteomyelitis.
Diagnostic imaging
Obtaining routine weight-bearing x-ray films of the foot can be considered for all patients when plantar heel pain is evaluated; generally, however, they are not helpful. Because heel spurs occur in about 15% of patients who do not have plantar fasciitis and in about 50% of patients who do,5 their presence is by no means diagnostic. In fact, the spur is not thought to be a cause of heel pain. However, stress fractures can be seen on lateral x-ray films.
Usually, bone scan results are abnormal in patients with plantar fasciitis because the origin of the plantar fascia is inflamed. Often, the scan confounds the diagnosis because the result is misinterpreted as a calcaneal stress fracture. Although bone scan results are abnormal in stress fractures, uptake occurs linearly in the body of the calcaneus.
Ultrasonography may show plan- tar fascia rupture or fibroma. CT scans can delineate tumors of the calcaneus; MRI can depict soft tissue tumors, stress fractures, and plantar fascia rupture as well as the thickening that occurs in cases of chronic plantar fasciitis. Electromyography and nerve conduction studies can document abnormalities of the tibial, medial plantar, and lateral plantar nerves. Electromyography does not often detect entrapment of the Baxter nerve.
Cases of tarsal tunnel syndrome accompanying plantar fasciitis are exceedingly rare. Usually, compression of the tibial nerve occurs only in cases in which there is a mass lesion. Tibial nerve symptoms associated with stretch neuropraxia resulting from foot pronation are most common; patients with this condition may have normal resting electrodiagnostic testing results. When inflammatory arthropathy is suspected, an arthritis laboratory profile should be obtained.
Conservative treatment
A minimum of 6 to 12 months of conservative treatment should be tried before surgery is considered; such treatment can be successful in at least 90% of patients.4,6,7 The nature of the treatment should be given stronger consideration than the duration. Poor conservative treatment provided indefinitely is unlikely to succeed; however, sound conservative measures are likely to resolve the patient's symptoms within a reasonable period.
Conservative treatment should address the inflammatory component that causes the discomfort and the biomechanical factors that result in the disorder. Treatment should include NSAIDs; wearing plantar fascia night splints and well-cushioned shoes, heel pads, or cups (or, in new-onset plantar fasciitis, off-the-shelf orthoses); and a vigorous program of plantar fascia and heel cord stretching. Patient education is imperative.
Splints and orthoses. Night splints that maintain the foot at an angle of 90° or more to the ankle have been used as adjunctive therapy; they prevent contraction of the plantar fascia while the patient sleeps. In one study, 83% of patients treated with such splints showed relief of recalcitrant plantar fasciitis pain.8 Gradually, resumption of running and sports can proceed after symptoms have resolved.
If symptoms have not resolved after 3 months, custom-molded orthoses can be considered. If a patient has significant plantar fasciitis pain resulting from a limb-length inequality or unilateral ankle equinus, a simple heel lift in the shoe of the affected foot may provide temporary relief.
The efficacy of a short leg walking cast in the management of chronic plantar heel pain was assessed for 32 patients with 37 involved extremities over a 2-year period.9 Of the 24 patients who had long-term follow-up, 10 (42%) were completely satisfied with cast treatment, 3 (12%) were satisfied but had reservations, and 11 (46%) were dissatisfied. In another study, a short leg cast worn for a minimum of 3 weeks was found to be effective for chronic plantar heel pain.10
Triceps surae stretching. Stretching is one of the easiest and most cost-effective conservative modalities. A major factor that contributes to plantar fasciitis is equinus. During gait, tightness within the Achilles tendon and gastrocsoleus complex results in compensatory increased dorsiflexion of the first MTP joint; this dorsiflexion stretches the plantar fascia at its insertion (the windlass effect). If the foot does not resupinate at toe-off, increased strain is placed on the plantar fascia.
Equinus also has been linked to increased foot pronation, which causes prolonged eversion of the calcaneus during gait, resulting in pathological stretching of the plantar fascia. Eventually, decreasing the tightness within the triceps surae with stretching will help ease plantar heel pain.
In a prospective randomized trial of nonoperative treatments of proximal plantar fasciitis, patients who underwent stretching exercises only (control group) had a 72% success rate.11 Pronation should be avoided during calf stretching because of the resultant compensatory mechanism of the unlocked midtarsal joint that destabilizes the foot; this decreases the effectiveness of the stretch and may increase the strain on the plantar fascia. Specific stretching of the plantar fascia may be as important as stretching of the heel cord.
Martin and colleagues12 conducted a study of 237 patients with plantar fasciitis to examine the effects on clinical outcome of a standardized treatment regimen and of patient compliance with various aspects of the regimen. The patients received 4-part nonoperative treatment that included NSAIDs, stretching exercises, night splints, and custom orthoses or heel cushions. More than 80% of patients were satisfied with the final outcome. Only 22% of patients received injections, and 10% of them consented to surgery. We concluded that stretching, night splints, and orthoses are equally useful and that good results can be obtained with nonsurgical treatment, but patients who have symptoms for more than 12 months have a lower chance of good outcome.
Corticosteroid injections. We believe that injections should be avoided in the initial treatment of patients with plantar fasciitis. They may provide only temporary relief and, if not used judiciously, they can result in loss of the plantar fat pad. We use injections only as supplemental treatment in patients who have resistant chronic plantar fasciitis and will be immobilized in a cam walker or short leg walking cast. Typically, 3 mL of an equal mixture of 1% lidocaine, 0.5% bupivacaine, and 1 mL of triamcinolone acetonide (40 mg/mL) is injected around the medial process of the calcaneal tuberosity. We have seen cases of plantar fascia rupture associated with injudicious use of corticosteroid injections in the heel.
Extracorporeal shock wave therapy (ESWT). ESWT generates pulses of high-pressure sound that travel through the skin. For reasons that are not fully understood, soft tissue and bone that are subjected to these pulses become less painful. The FDA has approved the use of some ESWT machines for heel pain and tennis elbow. The beneficial effect of the high-energy ESWT waves may be the result of growth of new blood vessels (neovascularization) in small cavities created by the pulses. Alternatively, the pulses may damage the deep sensory nerves, resulting in decreased pain. The average time to maximum improvement is 6 months.
In one study, the pain in patients with chronically painful proximal plantar fasciitis decreased by 64% to 88% on a visual analog scale 6 months after ESWT was initiated, and their comfortable walking time increased significantly.13 Weil and coworkers14 found that ESWT significantly reduces the symptoms associated with chronic plantar fasciitis and that the results compare favorably with those achieved with surgical intervention (percutaneous plantar fasciotomy).
In a study conducted to clarify the morphological features associated with the clinical outcome of chronic plantar fasciitis with ESWT, patients who had chronic plantar fasciitis with calcaneal bone marrow edema seen on pretherapeutic MRI had a satisfactory clinical outcome with ESWT.15 Typically, ESWT is performed as a single treatment; maximum improvement is achieved after 3 months.
Surgery
If extensive conservative treatment does not succeed, surgery may be indicated. Procedures include excision of a heel spur, complete or partial release of the plantar fascia,
osteotomy of the calcaneus, and drilling of the calcaneus. (For more on surgery for patients with heel pain, see Box, "Surgical approaches to plantar fasciitis.")
Although most authors have demonstrated a higher than 90% success rate with surgical procedures at short-term follow-up, none has discussed long-term biomechanical problems in the foot after release of the fascia. Kitaoka and coworkers16 suggested that operations involving fasciotomy affect arch stability and should not be performed on patients with evidence of concomitant pes planus deformity, because further deformation is likely. Therefore, surgery is best performed on those with normal and stable or high arches rather than those with flat feet.
All patients should be treated early with aggressive and appropriate conservative therapy. None should undergo early surgery except when there is nerve compression or entrapment; in these cases, surgical release for inferior heel pain is a good option.
References:
References1. Lester DK, Buchanan JR. Surgical treatment of plantar fasciitis. Clin Orthop Relat Res. 1984;186:202-204.
2. Bergmann JN. History and mechanical control of heel spur pain. Clin Podiatr Med Surg. 1990;7:243-259.
3. Barrett SL, Day SV, Brown MG. Endoscopic plantar fasciotomy: preliminary study with cadaveric specimens. J Foot Surg. 1991;30:170-172.
4. Amis J, Jennings L, Graham D, Graham CE. Painful heel syndrome: radiographic and treatment assessment. Foot Ankle. 1988;9:91-95.
5. Tanz SS. Heel pain. Clin Orthop Relat Res. 1963;28:169-178.
6. Davis PF, Severud E, Baxter DE. Painful heel syndrome: results of nonoperative treatment. Foot Ankle Int. 1994;15:531-535.
7. Malay DS. Plantar fasciitis and heel spur syndrome: a retrospective analysis. In: Vickers NS, ed. Reconstructive Surgery of the Foot and Leg-Update ’96. Tucker, GA: The Podiatry Institute; 1996:39-43.
8. Wapner KL, Sharkey PF. The use of night splints for treatment of recalcitrant plantar fasciitis. Foot Ankle. 1991;12:135-137.
9. Tisdel CL, Harper MC. Chronic plantar heel pain: treatment with a short leg walking cast. Foot Ankle Int. 1996;17:41-42.
10. Gill LH, Kiebzak GM. Outcome of nonsurgical treatment for plantar fasciitis [published correction appears in Foot Ankle Int. 1996;17:722]. Foot Ankle Int. 1996;17:527-532.
11. Pfeffer G, Bacchetti P, Deland J, et al. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int. 1999;20:214-221.
12. Martin RL, Irrgang JJ, Conti SF. Outcome study of subjects with insertional plantar fasciitis. Foot Ankle Int. 1998;19:803-811.
13. Hammer DS, Rupp S, Kreutz A, et al. Extracorporeal shockwave therapy (ESWT) in patients with chronic proximal plantar fasciitis. Foot Ankle Int. 2002;23:309-313.
14. Weil LS Jr, Roukis TS, Weil LS, Borrelli AH. Extracorporeal shock wave therapy for the treatment of chronic plantar fasciitis: indications, protocol, intermediate results, and a comparison of results to fasciotomy. J Foot Ankle Surg. 2002;41:166-172.
15. Maier M, Steinborn M, Schmitz C, et al. Extracorporeal shock wave application for chronic plantar fasciitis associated with heel spurs: prediction of outcome by magnetic resonance imaging. J Rheumatol. 2000;27:2455-2462.
16. Kitaoka HB, Luo ZP, An KN. Mechanical behavior of the foot and ankle after plantar fascia release in the unstable foot. Foot Ankle Int. 1997;18:8-15.
17. Baxter DE, Thigpen CM. Heel pain-operative results. Foot Ankle. 1984;5:16-25.
18. Barrett SL, Day SV. Endoscopic plantar fasciotomy for chronic plantar fasciitis/heel spur syndrome: surgical technique-early clinical results. J Foot Surg. 1991;30:568-570.
19. Snider MP, Clancy WG, McBeath AA. Plantar fascia release for chronic plantar fasciitis in runners. Am J Sports Med. 1983;11:215-219.
20. Silverman LM, Conti SF, Prasad A. Partial proximal plantar fasciectomy and release of the nerve to the abductor digiti minimi for recalcitrant chronic plantar fasciitis. Presented at: American Academy of Orthopaedic Surgeons 70th Annual Meeting; February 5-9, 2003; New Orleans.