Osteoarthritis: Has Oversimplification Led to Confusion?
One reason no good solution yet exists for osteoarthritis may be that rheumatology has been viewing many disease processes as a single entity. In an editorial, four rheumatologists offer a new disease model that they hope will rationalize future clinical research.
Castaneda S, Roman-Blas JA, Largo R, Herrero-Beaumont G. Osteoarthritis: a progressive disease with changing phenotypes. Rheumatology (2013) July (Epub ahead of print).
The tendency to view osteoarthritis (OA) as a single disease may be at the root of the medical profession's inability to solve the problem. OA is actually a complex of different disorders arising from numerous causes, observe the authors of this editorial in Rheumatology. These disorders are complicated by comorbidities. Left unresolved, all of them eventually culminate in a common syndrome of joint damage and, ultimately, replacement.
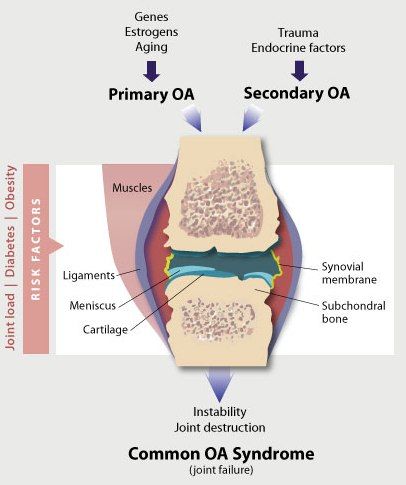
This is the thesis of rheumatologists from the Universidad Autonomia of Spain. They propose reclassifying primary OA into three subsets: type I (genetically determined), type II (estrogen-dependent), and type III (age-related). Complicated by the effects of joint loading, they add, altered adipokine activity and metabolic factors may exacerbate progression. Clinical phenotypes (bone injury, synovial inflammation, bursitis or tendonitis) depend on which tissue happens to be most damaged "at a given time," they say.
Treating osteoarthritis as a single disease "makes the outcome from current therapies disappointing," say Gabriel Herrero-Beaumont and his coauthors, because patients from different pathologic subgroups are treated identically. Future studies of osteoarthritis should be based on a better understanding of these subsets of disease, they add, and appropriate stratification of disease groups, especially in the case of patients with early OA.
The diagram above is adapted from one that appears in their article.