Patients and Physicians View Adherence Differently
Four recent studies have given physicians a more realistic picture of patient adherence to disease-modifying drug (DMD) treatments for multiple sclerosis (MS). Although study designs differed, all reported a disturbingly high level of nonadherence. The earliest study reported here is a survey of almost 800 MS patients from 17 neurology clinics in the US. Published in 2009, that survey found that 37% of patients admitted they had missed one or more injections of their DMD agent during the previous four weeks.
Looking at adherence from a different perspective, two studies published in 2011 analyzed prescription claims data to identify gaps in DMD treatment. Nonadherence was defined as a patient’s failure to obtain prescribed DMD drugs on a regular basis. Both analyses collected data over a two- to five-year period. Despite the differences in approach, number of patients, and timeframes, both database analyses were consistent with the earlier, patient-reported survey data:
• Halpern et al tracked DMD use by 6680 patients, finding that over time, adherence ranged from 52% to 62% in MS patients.
• Tan et al studied prescription data of 2446 patients, finding that 60% were adherent to DMD therapy.
Considering the importance of adherence in controlling progression of MS, another group of investigators returned to the survey approach in the hope of finding “why” and “how” so many patients are nonadherent. Researchersdesigned the MS Choices Survey, which surveyed prescribing physicians as well as patients. Results from this study, therefore, report two distinct points of view regarding adherence to DMD therapy. Supplying qualitative rather than quantitative results, the study sought information
that could be used by clinicians to improve patient adherence.
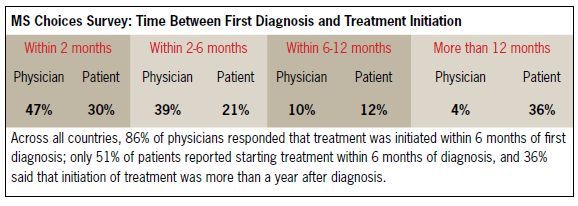
However, from the first question to the last, the answers from physicians indicated a much more positive, perhaps misguided, view of patient behavior. The patient responses did not support an assumption of early treatment initiation, or of adherence to DMDs. Almost all physicians (86%) reported that their patients initiated DMD therapy with 6 months of diagnosis. Among the patients who were surveyed, only half (51%) began DMD therapy within six months, and more than a third
(36%) waited for longer than a year. (Patients were not matched to a particular physician practice.)
Neurologists who were recruited for the survey had to have been in practice for three years or longer and had to see no fewer than 15 MS patients in an average month. It is possible that their patients were more closely followed than the group of patients answering the parallel survey. Still, the breadth of divergence between the group
responses to matched questions raises concerns.
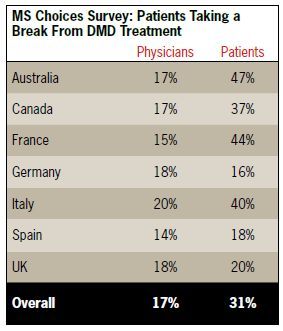
For example, responding physicians underestimated the number of MS patients who “decide to take a break” from their DMD therapy, as well as the number who discontinue therapy entirely. Across all countries, physicians estimated
that roughly 17% of MS patients take a break from treatment, and an average 14% discontinue therapy entirely. However, 31% of responding patients reported taking deliberate breaks from therapy, and 19% reported that they had stopped taking their MS treatment completely. And why? Eighty percent of physicians believe that the main
reason patients stop therapy is because of side effects. While 42% of patients agreed, checking “side effects” as a reason, that left more than half of the patient respondents viewing other factors as more personally difficult. The next largest group of patients reported that they took a break or discontinued using their DMD agent because they were “emotionally or mentally drained” or “fed up with therapy.” Others reported that they had “practical reasons to stop taking the therapy” or
the treatment “wasn’t working.”
The MS Choices Survey was fielded in seven countries: Australia, Canada, and five European countries. Although the breadth of divergence between physician and patient perceptions varied from country to country and also by question, the central conclusion is that physicians may underestimate the scale of poor adherence to DMDs as well as the reasons for it. If that is so, the physicians’ assessment of treatment efficacy might also be underestimated, and clinical decisionmaking about duration and escalation of therapies could be impacted. It also shows that some prescribing neurologists may be missing important opportunities to improve patient outcomes through a more direct, supportive dialogue with patients about adherence.
Sources
• Treadaway K, Cutter G, Salter A, et al. Factors that influence adherence with disease-modifying therapy in MS. J Neurol. 2009;256:568-576.
• Halpern R, Agarwal S, Dembek C, Borton L, Lopez-Bresnahan M. Comparison of adherence and persistenceamong multiple sclerosis patients treated with diseasemodifying therapies: a retrospective administrative claims analysis. Patient Prefer Adherence. 2011;5:73-84.
• Tan H, Cai Q, Agarwal S, Stephenson JJ, Kamat S. Impact of adherence to disease-modifying therapies on clinical and economic outcomes among patients with multiple sclerosis. Adv Ther. 2011;28:51-61.
• Riñon A, Buch M, Holley D, Verdun E. The MS Choices Survey: findings of a study assessing physician and patient perspectives on living with and managing multiple
sclerosis. Patient Prefer Adherence. 2011;5:629-643.
