PCI: New Imaging Detects Heart Attack Patients Who Don't Need It
About a quarter of patients who survived heart attacks due to blocked arteries could be treated with drugs, not invasive procedures. The trick is determining whether the blockage is cause by plaque erosion, not plaque rupture. With optical coherence tomography a team in Boston did just that.
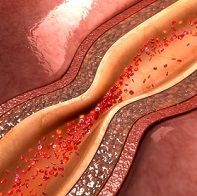
Stenting after a heart attack caused by an arterial blockage is generally effective but it is also expensive, invasive and comes with risks.
An estimated one quarter of patients who would normally be candidates for stenting might be spared the procedure if doctors had a way to learn if thei heart attack was caused by plaque erosion rather than plaque rupture.
In a study presented today at the European Society of Cardiology’s ESC Congress 2016 in Rome, Italy, Ik-Kyung Jang, MD, PhD, of Harvard Medical School, Massachusetts General Hospital in Boston, MA, said a new kind of cardiac imaging makes that possible.
Using an intracoronary imaging technique called optical coherence tomography (OCT) Jang and colleagues at Harvard and in China were able to deduce that in 405 patients in the study, more than a quarter of them (103 or 25.4%) had plaque erosion, which is generally treatable without stenting.
The new imaging was developed at Massachusetts Institute of Technology and scientists there are working to make their software widely usable at cardiac cath labs, Jang said in a news conference this morning.
The study, called EROSION, was simultaneously published in the European Heart Journal.
Jang said the patients were all in China but the COD analysis was done in Boston.
Of the 103 patients, 60 were judged eligible to take medications instead of getting a stent, based on criteria including having a residual diameter stenosis of less than 70% as shown in an angiogram and being stable without having symptoms.
The decision not to stent can be risky. One patient in the study died.
Still, Jang said at one month follow-up, 47 of these patients had smaller clots--at least 50% smaller than they had initially--and in 22% of these the clots were completely dissolved.
In addition to the patient who died while on dual antiplatelet therapy, one had to undergo PCI after showing no improvement.
Jang said the study was meant as a proof of concept, adding “We need a clinical trial and we are thinking about our next step.”
The procedure would be far safer and more feasible if patients with plaque erosion could be identified up front he said, with imaging then used to confirm the finding and guide therapy.
“Our hope is to find a biomarker for plaque erosion vs. plaque rupture,” he said.