Pigmented Villonodular Synovitis
PVNS is a rare, proliferative lesion of synovial tissue. This patient with a long history of knee pain recovered well after synovectomy.
A 44-year-old Hispanic woman was evaluated for a 1-day history of left knee pain and swelling. Two months earlier, the patient had started to walk as part of a weight loss program and had walked on a treadmill the day before the onset of pain. The pain was localized to the left knee, worsened with weight bearing, and was associated with swelling. There was no radiation of the pain, and no other joints were involved. The patient denied a history of fevers, chills, urinary symptoms, or recent trauma to the knee.
Nine years earlier, the patient had sustained an injury to her left knee while at work loading boxes onto a truck. Pain and swelling of the knee developed but resolved within 24 hours without intervention. Since then, the patient has had similar recurring episodes of the pain and swelling.
The patient's past medical history includes hypertension, hyperlipidemia, gastroesophageal reflux disease, and a pulmonary embolus. The only medication she had taken was a daily aspirin. The patient smokes cigarettes but has no history of alcohol use or recent travel.
On examination, there was a moderate effusion of the left knee, with mild warmth and tenderness. Range of motion was limited to 40° of flexion. The results of the remainder of her physical examination were normal. Plain radiographs showed increased density in the suprapatellar pouch, suggestive of effusion, with normal joint spaces.
The patient's left knee was aspirated, yielding 50 mL of yellow blood-tinged fluid. Synovial fluid analysis showed a white blood cell count of 2750/μL, with 77% neutrophils, and a red blood cell count of 7950/μL. No crystals were seen.
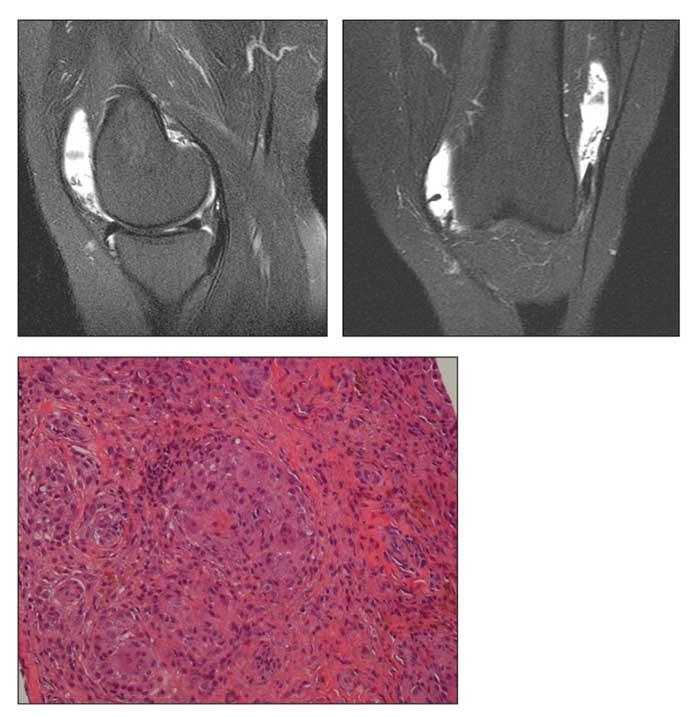
MRI scans and a microphotograph are shown.
The patient was referred to orthopedics for a diagnostic synovial biopsy. She underwent a left knee arthroscopy, which showed significant diffuse synovitis with yellow-brown pigmentation. A biopsy and synovectomy were performed. The patient's postoperative recovery was uneventful. She had full range of motion of the knee and had no pain on follow-up examinations. A diagnosis of pigmented villonodular synovitis (PVNS) was made.
PVNS is a rare, proliferative lesion of synovial tissue that occurs in 2 forms. The most common one is diffuse and involves the entire synovium. The other is localized and presents as a discrete mass within the synovium. Both forms may develop in intra-articular or extra-articular synovial tissue.
PVNS was first described by Chassaignac1 in 1852 as a nodular lesion from the flexor tendon synovial tissue of fingers. It had been referred to by several names until Jaffe and colleagues2 showed that all these entities had the same histological features and coined the term PVNS. An annual incidence of 1.8 cases per million persons was reported in a 1980 epidemiological study of 166 cases.3 An increased incidence is seen in persons aged 20 to 50 years; it rarely is reported in children.4
The cause of PVNS is unclear; most investigators favor a chronic inflammatory process. Some have suggested that PVNS may be a neoplastic process because it can metastasize, although rarely, and because there is evidence to indicate that some lesions are monoclonal.5,6 Various numerical and structural chromosomal abnormalities have been described.
PVNS is a locally aggressive lesion that almost always involves a single joint. The knees, hips, and fingers are most often affected, followed by the shoulders, feet, and ankles.7 PVNS of temporomandibular joint syndrome and of the spine have also been reported. The disease has an insidious onset and a slowly progressive course. Patients present with intermittent symptoms of pain, swelling, stiffness, and limited range of motion of the affected joint. Progressive disease may affect joint function.
Arthrocentesis may yield brown to bloody fluid or, rarely, blood.8 X-ray film results may be normal in the early stages, as in this patient, or demonstrate an increase in soft tissue density at the synovial sacs. Marginal erosions and cystic changes may be seen in one-third of chronic cases.8
CT scans are useful to demonstrate bone lesions; the synovium appears as a high-density mass because of increased iron content.9 However, MRI is the preferred method of imaging. It shows hyperplastic synovium, low signal intensity because of hemosiderin, and high signal intensity because of congested synovium and fat on T2-weighted images. Joint effusion is seen as low to intermediate signal on T1-weighted images and as high signal on T2-weighted images.
Surgical resection is the preferred method of treatment for diffuse and localized PVNS. Excision results in complete relief of symptoms without recurrences in localized PVNS.
Diffuse PVNS requires total or near total synovectomy by open method or by arthroscopy. Recurrence is common in diffuse PVNS, and the rate is similar with both surgical techniques.7
Low- to moderate-dose external beam radiation therapy is suggested for patients with residual disease or in patients with recurring disease.10 Infliximab and methotrexate have been shown to halt progression of persistent knee PVNS in a young patient with improvement in histology.11 Our patient was doing well at 5 months postsurgery without recurrence of pain or swelling of her knee.
References:
1. Chassaignac M. Cancer de la gaine des tendons. Gazette des Hôpitaux Civils et Militaires. 1852;47:185-186.
2. Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol. 1941;31:731-765.
3. Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: a clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore). 1980;59:223-238.
4. Vedantam R, Strecker WB, Schoenecker PL, Salinas-Madrigal L. Polyarticular pigmented villonodular synovitis in a child. Clin Orthop Relat Res. 1998;348:208-211.
5. Choong PF, Willén H, Nilbert M, et al. Pigmented villonodular synovitis: monoclonality and metastasis-a case for neoplastic origin? Acta Orthop Scand. 1995;66:64-68.
6. Ray RA, Morton CC, Lipinski KK, et al. Cytogenetic evidence of clonality in a case of pigmented villonodular synovitis. Cancer. 1991;67:121-125.
7. Chin KR, Barr SJ, Winalski C, et al. Treatment of advanced primary and recurrent diffuse pigmented villonodular synovitis of the knee. J Bone Joint Surg. 2002;84A:2192- 2202.
8. Flandry F, Hughston JC, McCann SB, Kurtz DM. Diagnostic features of diffuse pigmented villonodular synovitis of the knee. Clin Orthop Relat Res. 1994;298:212-220.
9. Al-Nakshabandi NA, Ryan AG, Choudur H, et al. Pigmented villonodular synovitis. Clin Radiol. 2004;59:414-420.
10. Ofluoglu O. Pigmented villonodular synovitis. Orthop Clin North Am. 2006;37:23-33.
11. Kroot EJ, Kraan MC, Smeets TJ, et al. Tumour necrosis factor alpha blockade in treatment resistant pigmented villonodular synovitis. Ann Rheum Dis. 2005;64:497-499.