Article
Preventing Catheter-Associated Urinary Tract Infection
Author(s):
The US Centers for Disease Control indicates more than 30% of healthcare-acquired infections reported by acute care hospitals are urinary tract infections (UTIs), making them the most common healthcare-associated infections.
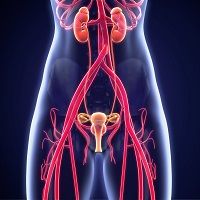
Buzz words come and buzz words go. CAUTI—Catheter-Associated Urinary Tract Infection—is currently high on the list of buzz words that concern hospital staff and management. The Joint Commission’s National Patient Safety Goals identify CAUTIs as serious hospital-acquired concerns. The US Centers for Disease Control indicates more than 30% of healthcare-acquired infections reported by acute care hospitals are urinary tract infections (UTIs), making them the most common healthcare-associated infections. Almost all CAUTIs follow urinary tract instrumentation.
Colorectal surgery (CRS) raises risk of postoperative infections including UTI enormously. A team of investigators from Carver College of Medicine at the University of Iowa has compared outcomes in CRS patients to patients with other medical and surgical hospitalizations. They looked at hospital charges, length of stay (LOS), and mortality after CRS at their institution. They found that CAUTI increased total hospital charges and LOS.
All hospitals track CAUTIs, and these investigators used their hospital’s quality surveillance data to identify post-colorectal resection-related UTI retrospectively. This area is somewhat complicated because hospitals use 2 definitions: the National Surgical Quality Improvement Program (NSQIP) definition of UTI, and the Centers for Disease Control and Prevention’s National Healthcare Safety Network (NHSN) definition of CAUTI.
The primary difference is that the latter requires the presence of an indwelling-urinary catheter. The investigators looked at any post-CRS infection that fit the UTI and CAUTI definitions.
Among 1124 patients who had CRS, 18 developed CAUTIs and 42 developed NSQIP-UTIs. This represents an overall UTI infection rate of 5.3%. Factors that increased risk of UTI included respiratory disease, age, male sex, and ASA class.
The overall mortality rate was 4.4%, and they found no link between either CAUTI or NSQIP-UTI. Patients who developed CAUTIs were significantly more likely to have longer LOS (the increase was 73%) and incur higher hospital charges (increased 70%).
This article is published in the Journal of Surgical Research.





