Article
Study: Optic Neuritis Changes Retinal Structure in MS Patients
Author(s):
A new study finds optic neuritis results in structural changes in the eye in MS patients, though it doesn’t appear to affect vision quality.
Patients with long-term multiple sclerosis (MS) and a history of optic neuritis experience significant structural neurodegeneration in their retinas, though the breakdown doesn’t appear to affect the quality of those patients’ vision.
Those are the findings of a Danish study published last month that looked at the structural impacts of optic neuritis (ON), a common problem for patients with MS. Some 40% of MS patients will develop optic neuritis during the course of their disease.
For 1 in 5 MS patients, optic neuritis is the presenting symptom that leads to an eventual MS diagnosis.
Study co-author Dr. Maria Rene Andersen, of the Department of Ophthalmology at the University of Odense, told MD Magazine that anecdotal evidence had suggested ON did not have long-term impacts on vision. This study helps confirm the observations empirically.
“The most important finding in our study was that although many patients had considerable and significant structural loss (of retinal nerve fiber layer) after an ON, visual acuity was preserved,” Andersen said. “This was not a complete surprise to us as in our clinic we often see that patients regain visual acuity and are without remaining visual symptoms after an ON.”
The study was additionally able to capture the long-term impacts of MS.
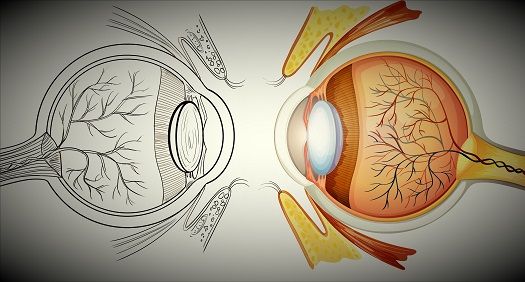
The research team looked at 82 patients who were diagnosed with MS between 2000 and 2006. The median age of the patient cohort was 49.9 and the number of years of MS duration at examination was 13, on average. Patients self-reported whether they had ever been diagnosed with ON. They were then given visual acuity and color vision tests, before undergoing spectra domain optical coherence tomography (OCT) to test structural markers of vision.
Of the 82 patients in the study, 23 had a history of ON. Researchers found that those patients tended to have reduced lower inferior and temporal RNFL thickness. The researchers also calculated that patients with RNFL thickness had 1.56 times a greater risk of ON versus patients without loss of RNFL thickness.
Aside from the results themselves, Andersen said the study also served as a demonstration of the usefulness of OCT “as a fast, non-invasive and cost-effective way of showing and quantifying structural RNFL-loss after ON in MS.”
The success of OCT in the study also brings to mind another possibility that researchers have been considering for some time: that OCT could be used as a tool to evaluate and diagnose different sub-types.
Previous studies have suggested that structural differences such as RNFL thickness could help physicians determine, for instance, if a patient has relapsing remitting MS, or whether it has progressed to secondary progressive MS.
Andersen said that question warrants additional study, but she said her research was designed with a different purpose in mind. It also didn’t have a sufficient population to answer such a question.
The study, “Long-term structural retinal changes in patients with optic neuritis related to multiple sclerosis,” was published in Clinical Ophthalmology last month.





