Suicide Rates Increased in 49 States Since 1999
The CDC reported that suicide rates have increased by at least 30% in half of all US states.
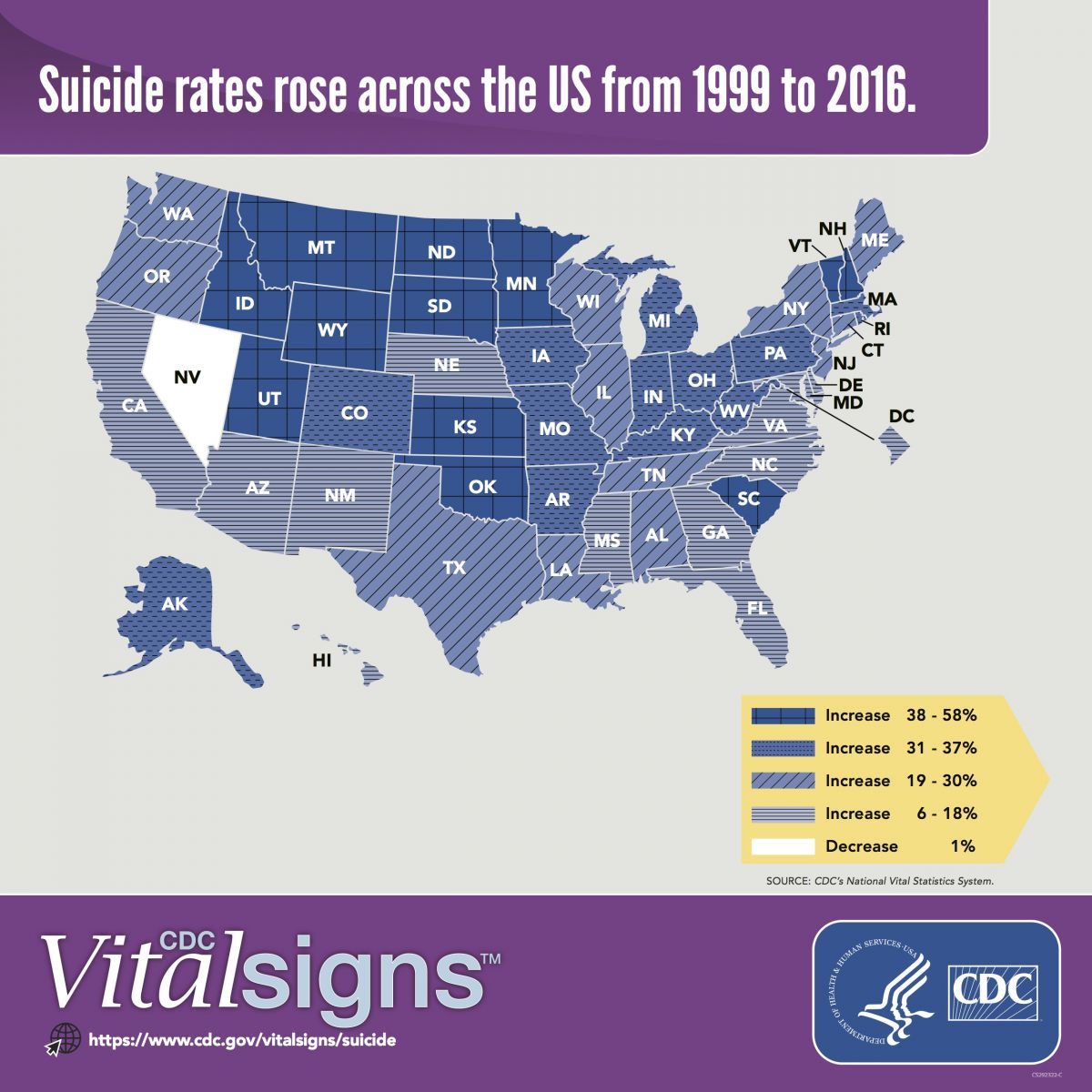
Courtesy of the US Centers for Disease Control and Prevention
A new report from the US Centers for Disease Control and Prevention (CDC) has shown that suicide rates are rising in nearly every state.
In an examination of state-level trends in suicide rates that ranged from 1999-2016, researchers from the CDC reported that rates increased by at least 6% in all states but Nevada, which reported a 1% decrease, in that span of time. Half (n= 25) of all states had suicide rate increases of at least 30%.
The increases were considered statistically significant in 44 of the states, with adjustments made for age, state, and sex across the 6 consecutive 3-year time periods observed. With considerations to gender, significant suicide rate increases were observed among males and females in 34 and 43 states, respectively.
Pulling data from the National Violent Death Reporting System (NVDRS) that observed contributing circumstances to suicide in decedents with and without known mental health conditions in 27 states in 2015, researchers reported that 54% did not have a known mental health condition. They found that relationship problems or loss (45.1% versus 39.6%), life stressors (50.5% versus 47.2%), and recent or impeding crises (32.9% versus 26%) were significantly more common among those without known mental health conditions than those with.
Suicide decedents without known mental health conditions were more likely to be male and non-Hispanic white than those with known mental health conditions. They were also more likely to commit a homicide followed by suicide (aOR = 2.9, 95% CI = 2.2—3.8) than the latter group.
Among decedents aged 18 years or older, 20.1% of those without known mental health conditions and 15.3% of those with had served in the US military.
Firearms were the most commonly reported method of suicides (48.5%), though decedents with known mental health conditions were less likely to die by firearm (40.6%) and more likely to use strangulation (31.3%) or poisoning (19.8%) than those without (26.9% and 10.4%, respectively).
With regards to regional suicide rate increases, the Midwest reported particularly significant numbers. Minnesota, North Dakota, South Dakota, Montana, Wyoming, Idaho, Utah, Kansas, and Oklahoma each reported increases from 38-58%.
This finding follows a 2017 CDC report that detailed the rise of suicide prevalence in rural US counties. In non-metropolitan areas, suicides were estimated to occur in 20 of every 10,000 residents in 2015.
Suicide has become a more prevalent topic among the US healthcare population in recent years, as well. A 2016 study of 100,000-plus medical students reported that more than 27% experienced depressive symptoms, and more than 11% have had suicidal thoughts. Experts in the field have speculated the reported rate of 1 in every 400 physicians committing suicide is an underestimate, pointing to differing death classifications in known cases.
The CDC is hoping future research delves into the specific causes of suicide trends, as NVDRS was capable of providing significant insight into decedent characteristics in more than half of the states.
“Suicidologists regularly state that suicide is not caused by a single factor; however, suicide prevention is often oriented toward mental health conditions alone with regard to downstream identification of suicidal persons, treatment of mental health conditions, and prevention of reattempts,” researchers wrote. “This study found that approximately half of suicide decedents in NVDRS did not have a known mental health condition, indicating that additional focus on non-mental health factors further upstream could provide important information for a public health approach.”
The study, "Vital Signs: Trends in State Suicide Rates — United States, 1999—2016 and Circumstances Contributing to Suicide — 27 States, 2015," was published online in the CDC's Morbidity and Mortality Weekly Report this week.