NIH: More Hydroxurea, Transfusions for Sickle Cell Patients
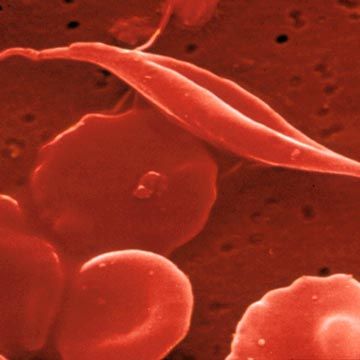
Doctors may be undertreating patients for sickle cell disease, a US National Institutes of Health (NIH) panel said. A group of experts convened by the NIH's National Heart, Lung, and Blood Institute issued new guidelines Sept. 9, calling for more aggressive treatment of these patients including periodic blood transfusions for pediatric patients. They also called strongly for greater use of hydroxyurea, a drug that promotes production of one type of healthy hemoglobin and thus dilute the amount of the faulty hemoglobin that causes the symptoms of sickle cells disease.
Doctors may be undertreating patients for sickle cell disease, a US National Institutes of Health (NIH) panel said.
A group of experts convened by the NIH’s National Heart, Lung, and Blood Institute issued new guidelines Sept. 9, calling for more aggressive treatment of these patients including periodic blood transfusions for pediatric patients.
They also called strongly for greater use of hydroxyurea, a drug that promotes production of one type of healthy hemoglobin and thus dilute the amount of the faulty hemoglobin that causes the symptoms of sickle cells disease.
In their recommendations, the panel noted that while hematologists are generally familiar with the treatments set out in the new guidelines, sickle cell patients are often seen by primary care providers, in outpatient settings, or in the emergency room.
The purpose of the new guidelines is to “support and expand the number of health professionals able and willing to provide care for persons with sickle cell disease,” the panel said.
The recommended therapies could not only relieve chronic suffering, but prevent hemoglobin from ”sickling” and causing the blockages in blood vessels and thickening of the blood that can cause crises like severe pain, organ damage, stroke and fatal complications.
Hydroxurea should play a major role in treatment, panel members agreed.
The drug encourages production of hemoglobin F, normally produced only during a person’s earliest development as a fetus. Having a higher level of healthy hemoglobin F also means a patient’s blood will have relatively less faulty hemoglobin.
When taken orally daily, the drug has been should to reduce or prevent any acute and complications of the disease.
“Hydroxyurea therapy substantially reduces the frequency of painful episodes and acute chest syndrome (ACS) events and the need for erythrocyte transfusions and hospitalizations,” the panel said.
Blood transfusions should also be used when pediatric patients appear to be at risk of stroke.
By adding normal hemoglobin in the donor’s blood, and thereby reducing the percentage of faulty hemoglobin in the patient’s blood, transfusions can reduce the chances children will have strokes, the experts said.
Hydroxurea can also head off acute chest syndrome (ACS) a common and dangerous complication of the illness, one that can send patients to the hospital. It usually presents as a sudden onset of coughing, shortness of breath and other respiratory symptoms. ACS is usually caused by an infection, but it can also be the result of an embolism in the bone marrow or clumps of sickled cells in the lungs.
“Long-term hydroxyurea administration results in a reduction in mortality.”
Many patients also need more treatment for pain.
An estimated 70,000 to 100,000 people in the US have the disease and about 3.5million carry the trait for it. The ailment is most common in African Americans. The disease shortens life expectancy by about 30 years.
The guidelines have more than 500 specific directions for physicians caring for these patients.
In Journal of the American Medical Association article on the new guidelines Barbara Yawn, MD, of the University of Minnesota, the co-chair of the NIH panel, said the group conducted an extensive review of literature and therapeutic trials to come up with its new recommendations.
But it also noted that the more than 12,000 documents it reviewed were all written in English, so it might have missed some foreign studies.
On the topic of health maintenance, the panel called for giving regular prophylactic doses of penicillin to newborns with the disease since children are at increased risk of invasive pneumococcal disease.
Patients should also get Hepatitis C screening since transfusions put them at risk for the virus.
The group also noted that pregnancy is risky for women with sickle cell disease, and their fetuses and newborns, but stopped short of saying these women should be counselling against having babies
. “Information on available contraception and reproductive issues in important” in caring for these women, the panel said.
There are also reproductive issues for men with the disease. About a third have episodic or chronic priapism—unwanted erections lasting at first a few hours but that can become almost constant.
The condition may respond to hormone therapy, but the panel said doctors should discuss treatment with these patients since hormones can also have unwanted side effects.