Article
4 Geographic Atrophy Drug Classes Under Development
Author(s):
A new review considered the progression of 4 treatment options being researched and developed for the treatment of the progressive form of vision loss.
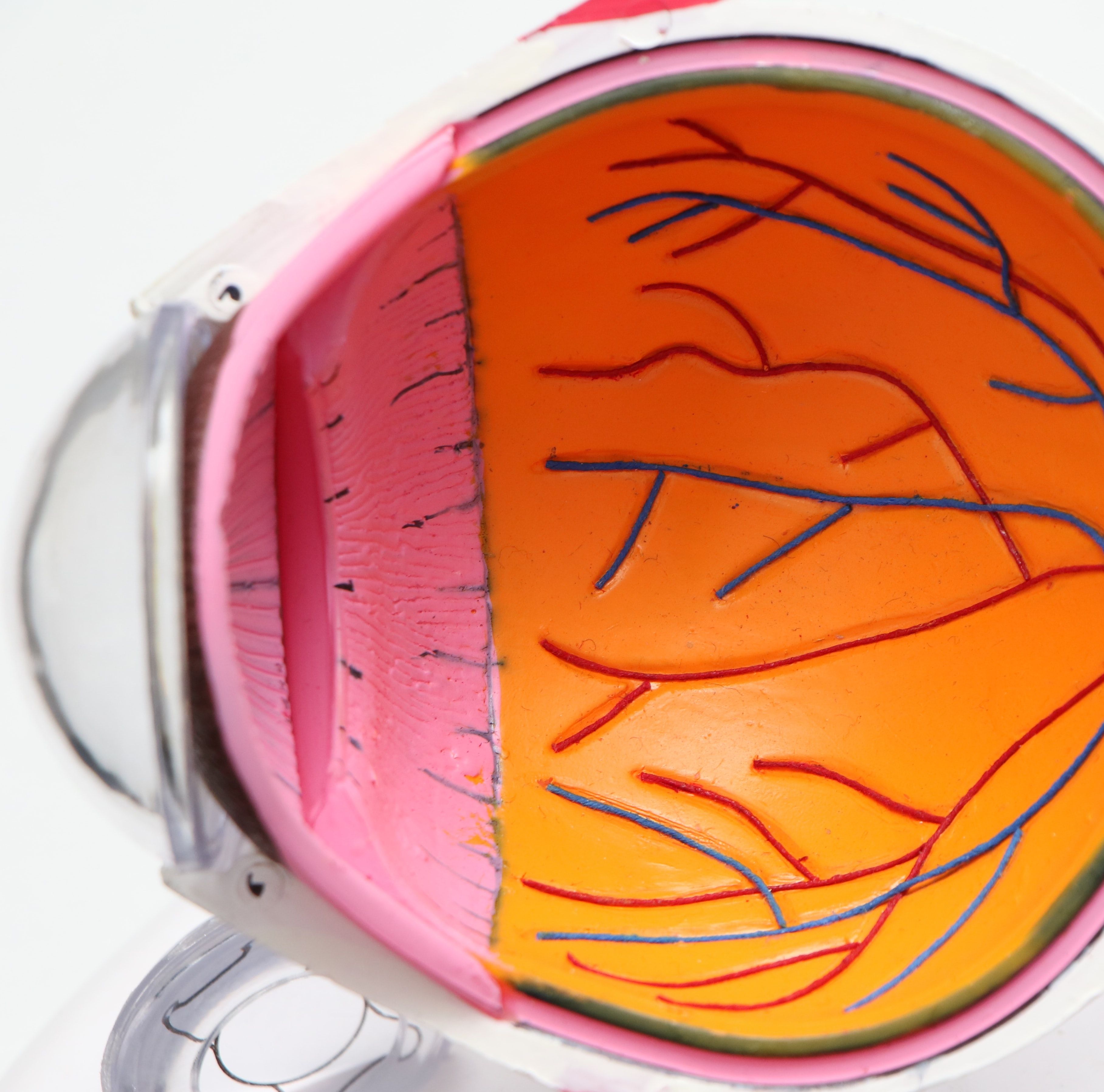
Credit: Unsplash / Harpreet Singh
Despite it representing the one of the most severe forms of age-related macular degeneration (AMD)—the most prevalent form of chronic vision loss among Americans—geographic atrophy remains a relatively unsolved clinical problem.
However, drug classes are in development—and as of last month, one has emerged on the market.
A recent review of the most promising treatment options for patients with geographic atrophy secondary to AMD—conducted by a team led by Hannah Khan, of the University of Nevada Reno School of Medicine—touched on a quartet of options reaching or nearing marketing indication to treat the burdensome ophthalmic disease.1
Complement Inhibitors
The immune response-targeting agents are the most developed in geographic atrophy clinical research—and are the first and only drug class to reach the market thus far.
Pegcetacoplan (SYFOVRE), approved by the US Food and Drug Administration (FDA) as the first drug indicated for geographic atrophy last month, inhibits all 3 complement system pathways.2 Its approval was based on positive results from the phase 3 OAKS and DERBY trials, wherein the injection therapy reduced the rate of lesion growth compared to sham and demonstrated increased treatment effects over 24 weeks. Data showed the greatest benefit of ≤36% reduction in lesion growth with monthly treatment in DERBY and occurred between 18 – 24 months.
The pivotal trial results additionally suggested a positive safety profile after approximately 12,000 injections. Results indicate the most common adverse reactions reported in patients receiving pegcetacoplan were ocular discomfort, neovascular AMD, vitreous floaters, and conjunctival hemorrhage.
Additionally in the later stage of clinical development is avacincaptad pegol, a pegylated RNA aptamer that binds to and inhibits cleavage of the complement C5 protein, which mitigates inflammation and geographic atrophy-associated cell death.
Avacincaptad pegol will be determined as a new FDA-approved drug by August. Its New Drug Application (NDA) is supported on 12-month, phase 3 data from the GATHER1 and GATHER2 clinical trials, in which the investigational agent provided efficacy per mean geographic atrophy growth rate of ≤35%.3
“Complement inhibitors have shown mixed results as therapeutic agents for the treatment of geography,” Khan and colleagues wrote. “Both avacincaptad pegol and pegcetacoplan have demonstrated meaningful reductions in GA lesion growth, while NGM621 unfortunately did not. Many therapeutics remain under investigation to delay disease progression and ultimately preserve macular function in patients with geographic atrophy.”
Neuroprotective Agents
As noted by the review team, neuroprotective agents potentially delay photoreceptor death in patients with geographic atrophy—thereby delaying disease progression. Their potential efficacy may be stringent on future assessments of neurotrophic factors, of which investigators need to better interpret their signaling cascades in order to prolong patients’ visual functions.
One agent, brimonidine, has been shown in mid-stage clinical trials capability to provide multi-mechanistic neuroprotection. The selective α2 adrenergic (α2A) receptor agonist was the subject of the phase 2 double-blind BEACON clinical trial, in which brimonidine intravitreal implant in patients with geographic atrophy secondary to AMD showed a mean 10% lesion reduction at month 24 and 12% at month 30 (P = .017), with favorable safety profiles without any unexpected adverse events.
Gene Therapies
The prospect of single-use gene therapies “may be a potential major advancement in retinal disease treatment,” wrote Khan and colleagues.
“Ocular gene therapy has demonstrated a favorable safety profile and offers a life-changing treatment option among patients with geographic atrophy,” they wrote. “Further investigations are necessary to optimize delivery methods, as well as further evaluating risks of chronic gene expression.”
Among leading candidates are GT005, an AAV2-based gene therapy designed to restore patients’ complement system homeostasis by increasing protein production, which would thereby reduce inflammation in patients.
The phase 1/2 FOCUS trial assessed 3 dose levels of GT005 in patients with geographic atrophy; 2 doses showed a positive safety profile, though mild adverse events were noted in patients’ study eyes. The ongoing phase 2 EXPLORE and HORIZON trials are assessing the one-time subretinal injection gene therapy based on genotyping to identify low protein production or a broader patient population.
“Evidently, an overactive complement system plays a pivotal role in dry AMD development, and subsequently, geographic atrophy disease progression,” reviewers wrote.
Another agent, AAVCAGsCD59, was designed to increase the soluble form of CD59, a cell surface protein that blocks MAC formation and thereby limits disease damage and atrophy. Its phase 1, dose-escalating HMR-1001 trial randomized 17 patients into 3 different arms of varying IVT dosage. Investigators observed a decreased rate of geographic atrophy progression in the highest-dose arm, though treatment was well tolerated in all 3 arms.
Stem Cell Therapies
The concept of stem cell therapy in treating geographic atrophy is relevant to the capability to achieve retinal pigment epithelium (RPE) and photoreceptor regeneration. One pertinent agent, OpRegen, is undergoing phase 1/2a assessment involving 24 participants divided into 4 cohorts.
Thus far, the human embryonic stem cell-derived RPE cell therapy has been associated with favorable safety signals and increased visual functions among treated patients. However, reviewers stressed the need for caution in the development and research of geographic atrophy stem cell therapy candidates—particularly in determining an appropriate cell type per patient.
“Safety and efficacy data, along with long-term clinical trial data are required to better equip ophthalmologists to incorporate this treatment option for geographic atrophy patients,” they wrote.
Furthermore, the reviewers concluded that the development of any geographic atrophy agents require ophthalmologists carefully consider all treatment options and their safety profiles to ascertain the absolute best efficacy for their patient.
“Improving the understanding of the pathophysiology of geographic atrophy secondary to dry AMD, for patients, optometrists, and ophthalmologists alike, may further aid in correctly identifying and diagnosing patients, reduce disease burden among patients, and ultimately, prolong their visual function,” they wrote.
References
- Khan H, Aziz AA, Sulahria H, et al. Emerging Treatment Options for Geographic Atrophy (GA) Secondary to Age-Related Macular Degeneration. Clin Ophthalmol. 2023;17:321-327. Published 2023 Jan 23. doi:10.2147/OPTH.S367089
- Iapoce C. FDA Approves Pegcetacoplan Injection for Geographic Atrophy. HCPLive. Published Feb 17 2023. https://www.hcplive.com/view/fda-approves-pegcetacoplan-injection-geographic-atrophy
- Iapoce C. FDA Accepts NDA for Avacincaptad Pegol for Treatment of Geographic Atrophy. HCPLive. Published Feb 17 2023. https://www.hcplive.com/view/fda-accepts-nda-avacincaptad-pegol-treatment-of-geographic-atrophy





