Advance in Tissue Engineering for Vision Loss
Non-destructive imaging and functional assessment of retinal structures formed from human stem cells confirms their similarity to the adult retina.
One obstacle to moving stem cells from the lab to the ophthalmology clinic has been an inability to view the structures these cells form and to assess how individual cells function in them without destroying them in the process. Because non-destructive imaging and functional assessment methods are needed to control cell quality and maximize production efficiency, these methods must be developed before stem cells can be used widely to treat retinal degeneration and screen eye drugs.
This week Andrew Browne, MD, PhD, of the Cleveland Clinic’s Cole Eye Institute reported on work he did last year at the University of Southern California (USC), Los Angeles. With Children’s Hospital of Los Angeles, Browne’s USC team tested several advanced methods for imaging retinal structures grown from human embryonic stem cells (hESC). Browne reported the results of these tests at the Association for Research in Vision and Ophthalmology (ARVO) Annual Meeting in Seattle, WA, on May 3, 2016. The team’s results were also published in an abstract included in the ARVO proceedings.
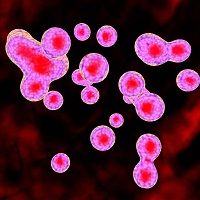
The development of retinal spheroids into sophisticated layered structures over time was the focus of the investigation. hESC can be induced to form such spheroids, which are composed of an empty core surrounded by several layers including a surface layer of photoreceptor cells. These spheroids are being developed for use in tissue engineering aimed at preventing or treating vision loss.
The researchers explored a range of imaging techniques that helped them to detect the structural changes that occurred in retinal spheroids as they developed. Each technique also provided insights on photoreceptor organization and metabolic activity. For example:
- Fluorescence Lifetime Imaging Microscopy (FLIM) allowed changes in metabolic activity to be detected over time. These changes were indicated by the free and bound amounts of the energy-generating chemical nicotinamide adenine dinucleotide + hydrogen (NADH). Although activity was initially similar throughout the spheroid, the outer retinal segments became very metabolically active as time progressed.
- Hyperspectral imaging (HSpec) showed the increase in retinol and retinoic acid concentrations in the spheroids’ active surface layers as the spheroids matured into organized layers.
- Three different ocular coherence tomography (OCT) devices were used to show the spheroids’ 3D structure and revealed a nuclear band after about 5 months of spheroidal development.
- Radiographic microcomputed tomography (microCT) allowed imaging of the spheroids at the micron level of resolution and provided intricate details on 3D structure.
- Immunofluorescence imaging confirmed the presence of the cone-rod homeobox (CRX), a marker for photoreceptors, on the spheroid’s surface.
Each of these methods produced results that correlated with those of standard hematoxylin and eosin histologic assessment. However, these methods were shown to provide more information than histologic assessment and brightfield microscopy.
Based on their investigations, the USC team concluded that “our retinal spheroids have both structure and metabolic activity that resembles the adult retina.” Their conclusion indicates that using stem cells for tissue engineering may become a successful approach to the prevention and treatment of vision loss.