Article
Anti-VEGF Agents better than no Anti-VEGF agents for AMD Patients
Author(s):
Investigators from Johns Hopkins examined 16 RCTs to determine efficacy of three anti-VEGF agents for patients with neovascular age-related macular degeneration.
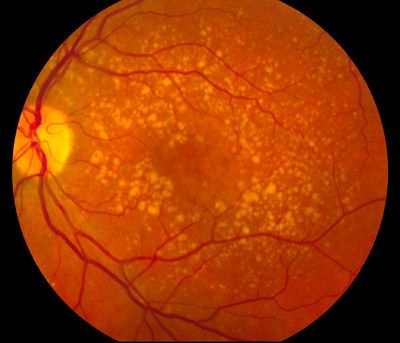
Anti-vascular endothelial growth factor (VEGF) agents such as pegaptanib, ranibizumab, and bevacizumab maintain visual acuity in patients with neovascular age-related macular degeneration (AMD), according to a new review.
Investigators found that patients with anti-VEGF agents were better than no aint-VEGF agents or other types of treatment for patients with wet AMD. In studies comparing anti-VEGF agents, the researchers found that ranibizumab and bevacizumab were similar in terms of vision-related outcomes and number of adverse events; the major difference was cost, as bevacizumab was cheaper.
Investigators, from Johns Hopkins University School of Medicine, sought to further investigate oculate and systemic effects of intravitreous injection of three anti-VEGF agents as well as their impact on quality of life. The investigators compared pegaptanib, ranibizumab, and bevacizumab compared to no anti-VEGF treatment in patients with AMD.
Investigators reviewed eligible studies from various literature databases and did not impose date or language restrictions on their search. They identified 16 randomized controlled trials through January 2018 with a total of 6347 participants diagnosed with AMD, though the participants per trial ranged from 23 to 1208. Of those 16 trials, 6 compared pegaptanib, ranibizumab, or bevacizumab to control treatment and 10 trials compared bevacizumab against ranibizumab.
The investigators determined that more patients who were treated with any of the anti-VEGF treatments compared to control subjects had gained 15 or more letters of visual acuity, had lost fewer than 15 letters of visual acuity and showed mean improvement of visual acuity after one year. In one pegaptanib trial, the investigators found a mean difference of 6.7 letters from 4.4 to 9.0. Among three ranibizumab trials, they found a mean difference of 17.8 letters from 16.0 to 19.7. Despite the lower cost of bevacizumab compared to ranibizumab, this remained true.Compared to control treatments, ranibizumab and bevacizumab treatments showed larger visual acuity outcomes than pegaptanib. No trial directly compared pegaptanib to another anti-VEGF agent.
Investigators found that AMD patients treated with ant-VEGF agents showed improvement in morphologic outcomes, including size of choroidal neovascularization and central retinal thickness, compared to those not treated with the agents. Central retinal thickness reduction was less among patients treated with bevacizumab compared to those treated with ranibizumab after one year, they added. Investigators added that the difference may not be clinically meaningful.
The most frequently reported serious ocular adverse events were ocular inflammation and increased intraocular pressure (IOP) after injection. Investigators reported endophthalmitis in less than 1% of anti-VEGF-treated patients and in no control patients. Serious systemic adverse events were comparable across treated and untreated patient cohorts. The varying study sizes might not be able to accurately depict meaningful differences between the group.
The investigators also found that researchers rarely measured and reported visual function, quality of life, or economic outcome data.
“Anti‐VEGF agents were better than no anti‐VEGF agents or other types of treatment for patients with wet AMD,” the study authors concluded. “When studies compared anti‐VEGF agents, researchers found that ranibizumab and bevacizumab were similar in terms of vision‐related outcomes and numbers of adverse events among participants followed for at least one year. The major difference was cost, as bevacizumab was cheaper.”
The paper, titled “Anti-vascular endothelial growth factor for neovascular age-related macular degeneration,” was published in the Cochrane Database of Systematic Reviews.





