Case Study: Debating Discontinuation of Disease-Modifying MS Therapies
Physicians debated the case of a 65-year-old woman with SPMS.

Is there a right time to discontinue disease-modifying therapies (DMTs) in MS management?
That point was up for discussion during the “Debates Over Controversies in Multiple Sclerosis” session at the Consortium of Multiple Sclerosis Centers Annual Meeting.
This debate was one among several case studies discussed by moderator Dennis Bourdette, M.D., co-director of the MS Center Excellence-West; Benjamin Segal, M.D., of the VA Ann Arbor Healthcare System; Olaf Stuve, M.D., PhD, of the VA North Texas Health Care System; and Mitchell Wallin, M.D., Director of the VA Center of Excellence-East. The debate took place on the meeting’s second day, Thursday, May 25, 2017.
Case 2 involved a woman with secondary progressive MS (SPMS) who asked to be taken off glatiramer acetate. The case details were as follows:
· “65-year-old woman with PhD presents for follow-up.
· Onset was in 2000 with numbness in feet for 1 month.
· Patient noted difficulties performing her research in early 2000s and in 2003 had recurrence of numbness in feet.
· Brain MRI showed changes consistent with MS; CSF showed elevated IgG index + OCB.
· Examination was normal.
· Started on glatiramer acetate in 2005.
· No relapses since 2005; brain MRI stable for at least past 5 years.
· Neuropsychology testing shows verbal fluency to be borderline low normal.
· Neurological exam remains normal.”
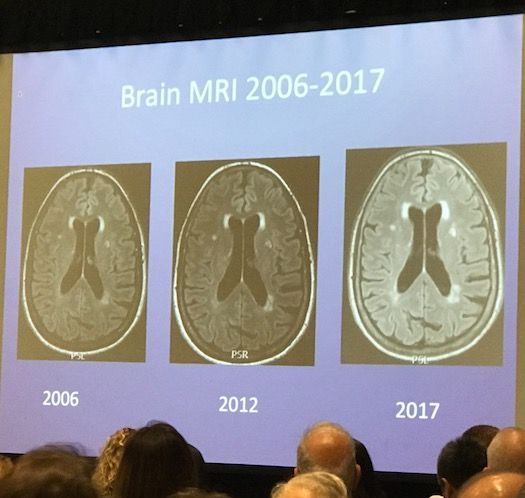
These are her Brain MRIs from 2006 to 2017:
Stuve took the position that the patient should stay on glatiramer acetate, but provided an overview of what he thought were the gray areas.
“This sure is a tough case,” Stuve said. “What we should think about is whether we should apply generalized criteria when we make a decision about cessation of therapy or not,” adding that the SPMS criteria are “somewhat crude.”
SPMS is always a retrospective diagnosis, Stuve said. If we had a biomarker for relapsing remitting MS (RRMS), there would be no gray area. He also added that all the physicians present had likely decided to discontinue DMTs in patients in the middle-aged group, only to have them relapse.
“It’s wrong to introduce criteria that simply use age for duration of therapy,” he said.
Stuve said that in some MS centers, physicians terminate DMTs at 50, and then observe the patient to see if it was a good decision. The potential problem in this approach is, “Is the patient stable because they transitioned to SPMS or because they responded to therapy?”
“We have to be careful making generalized decisions in patients with secondary progressive disease,” he said. “I think it’s wrong based on age and disease duration to discontinue therapy.”
Wallin took the position that the patient should be taken off the drug, noting that “the phenotype is somewhat challenging. He pointed out that the patient has gone 12 years without much disease activity, and that the neuro psychology testing does show a normal range, though it may be abnormal for someone of her intellectual caliber. Wallin said a physician could argue that the patient has benign MS and is asking a relevant question about discontinuation.
“It would be helpful to have more biomarkers and follow more closely for information,” Wallin said to Stuve’s point.
Citing a Swedish study on withdrawing DMTs that looked at stability in terms of routine sans and MRIS, Wallin said that 2/3 of the patients remained stable, with an annualized relapse rate of 0.12. There was, he said, no correlation between pre DMT and post-withdrawal relapse rate.
Wallin also pointed to a Gary Birnbaum study that followed 77 MS patients who had been stable for 2-20 years prior to ending their DMTs. In this study, 88% of the patients remained stable.
He said that withdrawal of first-line DMTs in older patients is relatively safe.
“I think, especially with someone in their mid ‘60s, it’s probably wise and judicious to take people off drugs that are not effective.”