Article
Decision Making in Upper Extremity Entrapment Neuropathies
A simple classification of nerve entrapment lesions separates candidates for a trial of conservative therapy from patients who will require referral for surgery.
ABSTRACT: Entrapment of the median, ulnar, and radial nerves in the upper extremity leads to a variety of syndromes. Physicians should have a thorough understanding of the causes, anatomy, diagnosis, and treatment options to provide patients with information for making effective decisions. The patient's occupational and recreational activities and comorbid medical conditions should be considered. The primary causative factor is mechanical compression of the nerve. Patient evaluation should start with a thorough history and physical examination, which may involve sensibility, provocative, and muscle strength testing. Diagnostic imaging and electrodiagnostic studies may help. A simple classification of nerve entrapment lesions separates patients who are candidates for a trial of conservative therapy from those who will require referral for surgery. (J Musculoskel Med. 2008;25:278-289)
Entrapment neuropathies are common, especially in the upper extremity, and may result in significant disability and morbidity. Entrapment of the median, ulnar, and radial nerves leads to a variety of syndromes. Patients may present with sensory disturbances of numbness, tingling, and pain in the distribution of the compressed nerve and motor dysfunction in the muscles supplied by the nerve. Pure pain, sensory, or motor syndromes or mixed syndromes may occur, depending on which nerve is affected.
The treating physician should have a thorough understanding of the causes, anatomy, and diagnosis of entrapment neuropathies, as well as the treatment options, to provide patients with the information needed to make the best decisions in managing their condition. Many factors play a role in the decision-making process; the patient's occupational and recreational activities and comorbid medical conditions should be considered, because they may affect the genesis or aggravation of nerve compression syndromes. Patients should be made aware of the natural history of their condition, especially if permanent neurological damage is a possibility when the condition is left unmanaged. In this article,we discuss the important decision-making factors.
PATHOPHYSIOLOGY
The primary causative factor in entrapment neuropathy is mechanical compression of the nerve. Normal anatomical structures along the nerve's path may be the source of compression (Table).
Potential sources of entrapment include a space with limited compliance, such as the carpal tunnel; proximity of the nerve to fibrous tendinous arches; and fascial bands. The nerve may be directly compressed along its course by abnormal anatomy that results from fractures, synovitis from rheumatoid arthritis, ganglion cysts, tumors, osteophytes, or aberrant muscles.
Chronic compression of the nerve leads to a pathological process that starts with obstruction of venous return. This process leads to segmental anoxia, capillary vasodilatation, and endoneurial edema, which compounds the compressive effects and leads to a disruption in axonal and cellular exchange.1 With prolonged compression, intraneural fibrosis and demyelination of nerve fibers begins; ultimately, it results in axonal degeneration. When the nerve cannot glide normally in its path, additional internal compression results from traction on the nerve.
Compression along the nerve may occur in more than 1 location (the "double-crush"phenomenon).2 Compression in a proximal location may disrupt axonal transport of nutrients essential for the survival and normal functioning of the axon, increasing the susceptibility of the distal axon to the effects of compression. For example, nerve compression in the cervical spine may increase the patient's propensity for carpal tunnel syndrome (CTS).
Patients with some comorbid medical conditions and personal risk factors also may be predisposed to compression neuropathies.3 These include anatomical factors (eg, bony abnormalities and neuromas); neuropathic, inflammatory, and congenital conditions and alterations of fluid balance; and position and motion factors (eg, vibration exposure, weight bearing with the wrist extended, and immobilization).
CLINICAL EVALUATION
Evaluation of patients with nerve entrapment complaints should start with a thorough history and physical examination. The duration and persistence of symptoms should be assessed. Controllable factors in the symptoms of nerve entrapment disorders may be indicated by the presence of comorbid conditions, an occupational and recreational history that involves postural or forceful repetitive motion factors, or substance use (eg, alcohol or tobacco). A history of trauma may point to fractures or dislocations as a cause of nerve compression and should elicit a quicker referral for surgical evaluation.
The physical examination is extremely important in evaluating patients; it may involve sensibility, provocative, and muscle strength testing. In sensibility evaluation in the distribution of the affected nerve, using Semmes-Weinstein monofilaments is valuable in quantifying the threshold of pressure sensation; comparison should be made with the unaffected nerves. Vibration testing may be used to assess the function of quickly adapting nerve fibers. For more severe cases, 2-point discrimination may be used to assess the density of innervation.
Provocative tests are specific to the nerve being tested. The goal is to elicit symptoms by irritating the nerve with maneuvers, such as wrist flexion, direct pressure, and percussion at the compression site.
Strength testing should be performed for the muscles supplied by the nerve in question; there are several specific tests for each syndrome. If muscle atrophy is observed, severe disease is present and referral for surgical treatment should be initiated. Regardless of the syndrome being considered, complete manual motor strength testing should be performed to rule out a cervical spinal cause of the neurological symptom or a more central cause.
Diagnostic imaging is useful in some cases. For example, a history of distal radius fracture may point to a malunion as the cause of median nerve compression; plain radiographs are indicated. MRI is useful if a tumor is suspected because ganglions and lipomas often cause compression, particularly in the forearm.
Electrodiagnostic studies, including electromyography (EMG) and nerve conduction velocity (NCV) testing, are useful for confirming the clinical diagnosis and defining the severity of nerve degeneration. EMG measures the response of muscle fibers to a conducted nerve impulse; NCV testing measures the speed of conduction of a nerve impulse. They are the only true objective tests of nerve dysfunction because they are independent of patient response during the examination. They also may help rule out cervical disk disease and polyneuropathy.
CLASSIFICATION
A simple classification of nerve entrapment lesions separates patients who are candidates for a trial of conservative therapy from those who will require referral for surgical evaluation. Mild disease has a duration of less than 1 year, with intermittent symptoms, normal 2-point discrimination, no muscle weakness or atrophy, no denervation potentials on EMG testing, and only mildly elevated NCV test results. In severe disease, patients have symptoms that persist for longer than 1 year, muscle weakness or atrophy, or marked abnormalities on electrodiagnostic studies; they should be referred for surgical evaluation. Surgery should be performed before patients become permanently weak or numb.
SPECIFIC SYNDROMES
Carpal tunnel syndrome
CTS, the most common compression neuropathy in the upper extremity, occurs as a result of compression of the median nerve as it passes through the carpal tunnel. Patients present with complaints of numbness, tingling, and pain in the thumb, index finger, middle finger, and radial half of the ring finger. They also may complain of clumsiness when handling objects or a feeling of fatigue in the hand (resulting from weakness of the thenar muscles). Nocturnal paresthesia and pain are common; these symptoms often awaken patients, prompting them to shake the hand to relieve their symptoms.
Physical examination may reveal changes in the Semmes-Weinstein pressure threshold, vibratory threshold, or 2-point discrimination in the radial 3¹⁄? digits. Thenar muscle strength may be tested as shown in Figure 1; thenar muscle atrophy indicates severe, prolonged compression of the nerve. The Durkan and Phalen provocative tests are shown in Figure 2. The Tinel sign is performed by percussing along the course of the median nerve; the result is positive if paresthesia is reproduced in the median nerve distribution.

Figure 1 –
In evaluation of patients for carpal tunnel syndrome, thenar muscle strength is tested by placing the patient's hand flat on the examination table with the palm facing up. The patient is then asked to raise the thumb off the table against resistance; this tests abduction strength, which is purely median nerve innervated. The thenar muscle mass is palpated simultaneously to assess muscle contraction and muscle atrophy.
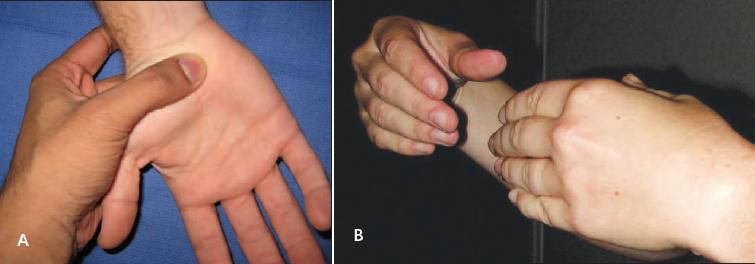
Figure 2 –
The Durkan median nerve compression test is the most sensitive physical test for detecting carpal tunnel syndrome. The examiner performs the test by applying direct pressure on the median nerve at the carpal tunnel with his or her thumb (A). The result is positive if symptoms appear within 30 seconds and disappear when pressure is released. In performing the Phalen wrist flexion test (B), eliminate elbow flexion to prevent compression of the ulnar nerve at the cubital tunnel; compression may produce symptoms in the small and ring fingers. The result is positive if symptoms are reproduced after the wrist is held in a flexed position for 60 seconds or less.
Radiography is useful if there is a history of fracture or dislocation of the carpal bones or distal radius, wrist arthritis, or a detectable mass on physical examination. X-ray films should be obtained if the physical examination shows decreased wrist flexion or extension. Electrodiagnostic studies confirm the clinical diagnosis and quantify disease severity.
Treatment for patients with CTS varies with disease severity and chronicity. If the patient's condition is mild, 6 weeks to 3 months of nonoperative management can be started. A systematic literature review showed that splinting, oral corticosteroids, and ultrasonography have reasonable short-term benefits4; however, long-term results are still unproved. Corticosteroid injection may improve symptoms for up to a month but also does not appear to have longterm benefits.5 However, offering nonsurgical management options to patients who have only mild disease is reasonable.
Surgery candidates include patients with CTS symptoms that persist despite conservative treatment and those with severe disease characterized by persistent symptoms for more than 1 year, muscle weakness or atrophy of the thenar musculature, or marked abnormalities on electrodiagnostic studies. Surgery may involve a variety of approaches, including open and endoscopic techniques. Success may be achieved with both techniques, and there is no demonstrable advantage of one release over the other.6
Overall, surgical treatment halts disease progression and improves patient symptoms more reliably than nonoperative treatment. In advanced cases, symptoms may not resolve completely after surgical release.
Pronator syndrome
Compression of the median nerve in the proximal forearm may result in pronator syndrome, which occurs less frequently than CTS. As the nerve travels down the upper extremity it passes several anatomical structures that may become sites of compression.
Pronator syndrome presents as forearm pain, along with paresthesia and numbness in the median nerve distribution, similar to that seen in CTS. Numbness in the thenar eminence at the base of the thumb is found (unlike in CTS) because the palmar cutaneous branch of the median nerve, which innervates the thenar eminence, branches proximal to the carpal tunnel. Symptoms often are exacerbated with activity, especially that requiring repetitive elbow flexion-extension or pronosupination. Nocturnal symptoms, such as those seen in CTS, are uncommon.
The physical examination consists of thorough sensibility testing. Motor weakness usually is not present. Performing the Tinel sign at the proximal forearm produces paresthesia in the distribution of the median nerve. The Phalen test result is negative.
Radiographs, including an oblique view of the elbow, help rule out a supracondylar process (a bone spur and ligament complex that may be an anatomical site of compression). Electrodiagnostic test results are positive for pronator syndrome in only up to 50% of patients, but they are useful in the differential diagnosis by ruling out CTS, cervical radiculopathy, and polyneuropathy.7
Pronator syndrome typically involves pain and paresthesia but not motor changes. Therefore, treatment typically is nonoperative, especially if the symptoms are of short duration. Conservative treatment results in resolution of symptoms in 50% of patients.8 Splinting is effective; a removable long-arm splint is used with the elbow in 90° of flexion, the forearm in slight pronation, and the wrist in slight flexion. Anti-inflammatory medications may be used for symptomatic relief; corticosteroid injections play no role in this syndrome.
Patients for whom nonoperative treatment has not been successful for up to 3 months are candidates for surgical release of the entire course of the proximal median nerve. Up to 92% of patients who undergo surgical release report good or excellent results.7
Anterior interosseous nerve (AIN) palsy
The AIN is the largest branch of the median nerve; it may be compressed by the same structures in the proximal forearm as in pronator syndrome.The AIN usually innervates the flexor digitorum profundus to the index and middle fingers, the flexor pollicis longus, and the pronator quadratus; however, there are several anatomical variations.
Patients with AIN palsy may present initially with complaints of vague pain in the proximal forearm that is exacerbated by activity. The diagnosis is made by finding weakness in the muscles that the AIN innervates. Patients may have difficulty in writing and other activities that require tip pinch activity because of weakness in AIN-supplied muscles.
In AIN palsy, the thumb and index finger assume a characteristic position with pinching. Pronator quadratus strength may be tested by having the patient attempt to pronate against resistance with the elbow in flexion to eliminate the effect of the pronator teres. Sensation is not affected.
Physicians should differentiate compression neuropathy from Parsonage-Turner syndrome (PTS), a brachial plexus neuritis that may affect the AIN and may have a similar presentation. The distinction is made primarily with the patient's history. PTS is associated with a history of pain in the arm, elbow, or forearm that precedes the motor symptoms of AIN palsy. It may be spontaneous or occur after a viral illness, vaccination, or unrelated surgical procedure (eg, appendectomy or meniscectomy).9 In contrast, compression neuropathy may be associated with a history of acute or repetitive trauma; usually there is no preceding arm or elbow pain aside from that associated with trauma.
Electrodiagnostic test results may be identical in the 2 syndromes. Performing shoulder girdle EMG testings is important because the results may be positive initially in cases of PTS and often are overlooked by the uninitiated as incompatible with isolated motor weakness in the hand. MRI of the brachial plexus also may help distinguish brachial neuritis from AIN compression.10
When AIN palsy is the result of true compression, surgery is indicated. Because a definitive diagnosis is not always immediately possible, initial treatment typically is nonoperative, with immobilization and monitoring in spite of motor involvement. Success rates of up to 90% may be achieved, but resolution may take up to 18 months and may not be complete.11 A trial of nonoperative treatment is a reasonable approach for up to 4 to 6 months. If there are no clinical or electrophysiological signs of improvement, the patient should be referred for surgical decompression; success rates are about 90%.12
Cubital tunnel syndrome (CBTS)
This syndrome, caused by entrapment of the ulnar nerve at the elbow, is the second most common entrapment neuropathy in the upper extremity. Repeated elbow flexion or direct compression of the ulnar nerve at the elbow may increase pressure within the cubital tunnel. Ulnar nerve subluxation also contributes to the condition. Several anatomical structures can entrap the nerve. Potential causes include trauma with resulting malunion or deformity, medial elbow instability, tumors, and aberrant muscle.
Patients with CBTS may complain of paresthesia and numbness in the small finger and the ulnar half of the ring finger with aching pain in the medial elbow and proximal forearm. Nocturnal symptoms may awaken the patient. With severe disease, patients may have weakness of the intrinsic muscles of the hand that affects their grip strength and decreases dexterity.
Sensibility testing results may be abnormal in the small finger and the ulnar half of the ring finger and on the dorsoulnar part of the hand. Key pinch strength is tested to assess the motor component of the nerve.
Clawing of the small and ring finger and wasting of the interosseous muscles and hypothenar eminence are signs of severe disease. In advanced cases, patients have weakness of their long digital flexors (flexor digitorum profundus) to their little and ring fingers and ulnar wrist flexor (flexor carpi ulnaris). Provocative tests include the Tinel sign over the cubital tunnel and the elbow flexion test; the result of the latter is positive if paresthesia is reproduced with elbow flexion within 30 seconds.
Radiographs are obtained if there is a history of elbow trauma or arthritis. Electrodiagnostic tests help distinguish between CBTS and ulnar tunnel syndrome (UTS), as well as cervical spine disease.
Mild cases may be managed with nonoperative measures. Up to 90% of patients do well; symptoms resolve within 2 to 3 months.13 Patients should be educated about avoiding activities that require repetitive or prolonged elbow flexion or leaning on the elbow. Effective nonsurgical approaches include night splinting with the elbow in 45° of flexion and neutral forearm rotation and the use of soft elbow pads.
Candidates for surgical treatment include patients for whom conservative treatment is not successful and those with moderate to severe disease with evidence of motor involvement. There are several surgical options, including simple nerve decompression, 3 methods of nerve transposition, and medial epicondylectomy. In the literature, no single procedure has been shown to be more effective than the others; however, the overall results are excellent when surgery is performed before the disease becomes severe.14
Ulnar tunnel syndrome
This rare condition is caused by compression of the ulnar nerve at the wrist as it passes through the Guyon canal. Compression at this level usually is the result of a space-occupying lesion, hook of hamate fracture, or repetitive trauma to the hypothenar region. Bicyclists may have symptoms resulting from prolonged pressure on the hypothenar area of the palm. The most common lesions include ganglia, pseudoaneurysms, ulnar artery thrombosis, and anomalous muscles. In the Guyon canal, the ulnar nerve splits into a deep motor branch that innervates the intrinsic and hypothenar muscles and a superficial branch that is primarily sensory but also innervates the palmaris brevis. Lesions at this location may cause purely motor, purely sensory, or mixed symptoms.15
Patients may present with sensory and motor symptoms that are similar to those in CBTS. However, the dorsoulnar part of the hand is unaffected in UTS because the dorsal cutaneous branch of the ulnar nerve branches before the Guyon canal.
On physical examination, the Tinel sign is positive at the wrist but not at the elbow. Elbow flexion provocation results are negative. Palpation over the tunnel may reveal a mass that may be pulsatile, as in the case of ulnar artery thrombosis. Motor testing results are similar to those in CBTS, but the flexor carpi ulnaris and flexor digitorum profundus results are always normal in UTS.
Electrodiagnostic testing also may help localize the lesion and distinguish UTS from CBTS. If UTS is suspected, radiographs-including a carpal tunnel view-help rule out hook of hamate fractures. MRI may help detect masses within the Guyon canal; CT would show a hook of hamate fracture.
Treatment for patients with UTS compression usually is surgical because the disorder is most often caused by an anatomical lesion.16 Excision of the mass or a symptomatic hook of hamate fracture may be needed.
Posterior interosseous nerve (PIN) syndrome
PIN entrapment may result in 1 of 2 distinct entities, PIN syndrome or radial tunnel syndrome (RTS). PIN syndrome presents with a purely motor deficit exhibited by weakness in the finger and thumb extensors and the extensor carpi radialis brevis. Active wrist extension is possible, but the wrist may deviate radially with extension because of unopposed action of the extensor carpi radialis longus, which is innervated by the radial nerve before PIN branching.
Distinguishing muscle weakness from tendon rupture is important. This can be accomplished by using the tenodesis effect; as the wrist is passively flexed, intact extensor tendons extend the digits. Sensory changes usually are not part of this syndrome.
The most common causes of PIN syndrome are space-occupying lesions, such as lipomas and ganglions; trauma; and rheumatoid synovitis. Therefore, plain radiography and MRI are useful in looking for masses, malunion, or osteophyte formation. Electrodiagnostic test results are positive, and the tests help establish the location of the lesion.
If there are space-occupying lesions, surgical treatment is indicated. If the workup does not reveal a lesion, a short course of nonoperative treatment with rest and splinting may be attempted for up to 3 months. If symptoms progress or do not improve, surgical treatment is advised; outcomes often are favorable.17
Radial tunnel syndrome
PIN compression also may result in a more controversial diagnosis, RTS. Compression sites in RTS are identical to those in PIN syndrome. However, there is no muscle weakness; dull aching in the extensor-supinator mass at the lateral forearm is the primary complaint.
Distinguishing RTS from lateral epicondylitis may be difficult. In RTS, symptoms are exacerbated by activities that require repetitive elbow flexion-extension or pronosupination; lateral epicondylitis presents with sharp pain at the lateral epicondyle that is exacerbated with activities requiring wrist extension. The conditions may coexist, increasing the diagnostic challenge.
On examination, patients with RTS have tenderness in the extensor-supinator mass in the proximal forearm; patients with lateral epicondylitis usually have tenderness at or slightly anterior to the lateral epicondyle. Resisted forearm supination or resisted middle finger extension may exacerbate the pain associated with RTS; pain with resisted wrist extension is characteristic of lateral epicondylitis. Patients often report subjective weakness because of limitation resulting from pain, but objective weakness is not found.
The diagnosis of RTS is clinical; imaging and electrodiagnostic testing rarely are useful. If pain relief occurs, injection of a few milliliters of 1% lidocaine into the radial tunnel may help confirm the diagnosis. Weakness of PIN-innervated muscles after injection verifies that the injection was performed properly.
If there are no objective motor findings, the mainstay of treatment is nonoperative. Rest, splinting, use of anti-inflammatories, and avoidance of aggravating activities may relieve symptoms.
References:
References
1.
Lundborg G, Myers R, Powell H. Nerve compression injury and increased endoneurial fluid pressure: a “miniature compartment syndrome.”
J Neurol Neurosurg Psychiatry.
1983;46:1119-1124.
2.
Upton AR, McComas AJ. The double crush in nerve entrapment syndromes.
Lancet.
1973;2:359-362.
3.
Szabo RM, Madison M. Carpal tunnel syndrome.
Orthop Clin North Am.
1992;23:103-109.
4.
O’Connor D,Marshall S, Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome.
Cochrane Database Syst Rev.
2003;(1):CD003219
5.
Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome.
Cochrane Database Syst Rev.
2007;(2):CD001554.
6.
Scholten RJ, Mink van der Molen A, Uitdehaag BM, et al. Surgical treatment options for carpal tunnel syndrome.
Cochrane Database Syst Rev.
2007;(4):CD003905.
7.
Hartz CR, Linscheid RL, Gramse RR, Daube JR. The pronator teres syndrome: compression neuropathy of the median nerve.
J Bone Joint Surg.
1981;63A:885-890.
8.
Johnson RK, Spinner M. Median nerve compression in the forearm: the pronator tunnel syndrome. In: Szabo RM, ed.
Nerve Compression Syndromes-Diagnosis and Treatment.
Thorofare, NJ: Slack Incorporated; 1989:137-159.
9.
Malamut RI, Marques W, England JD, Sumner AJ. Postsurgical idiopathic brachial neuritis.
Muscle Nerve.
1994;17:320-324.
10.
Bredella MA, Tirman PF, Fritz RC, et al. Denervation syndromes of the shoulder girdle: MR imaging with electrophysiologic correlation.
Skeletal Radiol.
1999;28:567-572.
11.
Hill NA, Howard FM, Huffer BR. The incomplete anterior interosseous nerve syndrome.
J Hand Surg.
1985;10A:4-16.
12.
Kim DH, Murovic JA, Kim YY, Kline DG. Surgical treatment and outcomes in 15 patients with anterior interosseous nerve entrapment and injuries.
J Neurosurg.
2006;104:757-765.
13.
Mowlavi A, Andrews K, Lille S, et al. The management of cubital tunnel syndrome: a meta-analysis of clinical studies.
Plast Reconstr Surg.
2000;106:327-334.
14.
Zlowodzki M, Chan S, Bhandari M, et al. Anterior transposition compared with simple decompression for treatment of cubital tunnel syndrome: a meta-analysis of randomized, controlled trials.
J Bone Joint Surg.
2007;89A:2591-2598.
15.
Gross MS, Gelberman RH. The anatomy of the distal ulnar tunnel.
Clin Orthop Relat Res.
1985;196:238-247.
16.
Waugh RP, Pellegrini VD Jr. Ulnar tunnel syndrome.
Hand Clin.
2007;23:301-310.
17.
Kim DH, Murovic JA, Kim YY, Kline DG. Surgical treatment and outcomes in 45 cases of posterior interosseous nerve entrapments and injuries.
J Neurosurg.
2006;104:766-777.




