Article
Diagnosing Tuberous Sclerosis Complex Before Seizure Onset
Author(s):
Results from a study recently published in the Orphanet Journal of Rare Diseases confirms the idea that tuberous sclerosis complex (TSC) can be diagnosed before seizure onset.
Results from a study recently published in the Orphanet Journal of Rare Diseases confirms the idea that tuberous sclerosis complex (TSC) can be diagnosed before seizure onset.
Monika Slowinska M.D. of the Department of Neurology and Epileptology at The Children’s Memorial Health Institute, Warsaw, Poland and her team of researchers performed a retrospective review of children who were suspected of having TSC due to single or multiple cardiac tumors as the initial presentation of the disease, born between 1990 and 2016. The medical records, in terms of conducted clinical tests and TSC symptoms — which were observed until the 4th month of age — were analyzed throughout the study.
TSC is characterized by the uncontrolled growth of benign tumors in multiple organs, including the brain, kidneys, heart, lungs, eyes, and skin. While symptoms vary from patient to patient, seizures are the most common among the population. The study’s purpose was to define the most useful approach to make a TSC diagnosis before seizure onset (before the age of 4 months), so that early Electroencephalography (EEG) monitoring with possible preventative treatment intervention could be conducted.
In the analysis, 100 children were identified, 82 of whom were diagnosed with TSC within the first 4 months of life.
68 children from the Department of Neurology and Epileptology of The Children’s Memorial Health Institute of Warsaw were evaluated, along with 32 children from Child Neuropsychiatry Unit and Epilepsy Center of the San Paolo Hospital in Milan. The study group was divided into 3 cohorts: patients with ‘early diagnosis,’ established until the end of 16 weeks of age; patients with ‘late diagnosis,’ made after 16 weeks of age; and patients with ‘possible TSC,’ in whom the diagnosis was not confirmed.
Medical records in terms of clinical tests that were conducted and TSC diagnostic signs that were observed within 16 weeks of life were analyzed, and the diagnostic criteria according to recent recommendations from the Tuberous Sclerosis Consensus Conference in 2012 were applied. The diagnosis of TSC was confirmed in children with at least 2 major criteria or 1 major and 2 minor, or when a pathogenic mutation in either TSC1 or TSC2 was identified.
Results of the study showed that early diagnosis of TSC, before clinical seizure onset, is possible. In 82% of patients evaluated, the diagnosis was established before the end of the 16th week of life, which is regarded as the typical time of clinical seizure onset. Clinical seizures are preceded by EEG abnormalities; thus, regular EEG surveillance and early implementation of antiepileptic treatment is clinically beneficial for developmental outcome and seizure control.
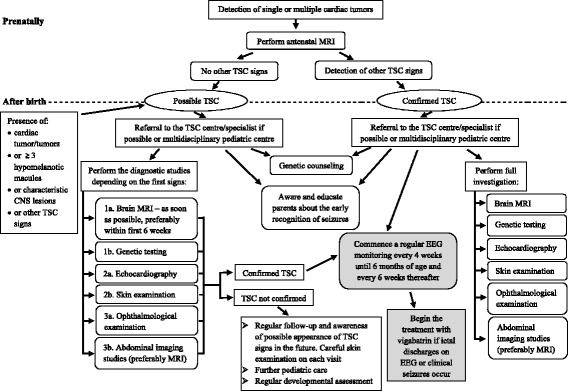
Figure 1 (below) proposes the diagnostic and management algorithm necessary for early TSC diagnosis:
The data of seizure onset and developmental outcome were not analyzed in the cohort, and only children in whom the first sign of disease was cardiac tumors were included.
For more on studies evaluating the diagnosis of patients in the rare disease community, follow Rare Disease Report on Facebook and Twitter.
Sources:
1. Slowinska M, Jozwiak S, Peron A, Bertamino A, Borkowska J, et al. Early diagnosis of tuberous sclerosis complex: a race against time. How to make the diagnosis before seizures? Orphanet Journal of Rare Diseases. 2018:13-25. doi: 10.1186/s13023-018-0764-z.




