Article
Gut Microbiota Dybiosis May Be Linked to Rheumatic Disease
Author(s):
Developing research into the specific alterations of dysbiosis and diseases like arthritis suggest possibly novel pathways to therapy development.
A new assessment observed an association between rheumatic disease and gut microbiota dysbiosis.
Systematic review and meta analysis data from a team of investigators in China showed a correlation of potentially nonspecific, shared alterations of gut microbes in patients with either dysbiosis or rheumatic diseases including arthritis and systemic lupus erythematosus (SLE).
The findings contribute further evidence to a proposed link between the 2 disease group pathologies, and provide clearer paths for follow-up research.
Led by Yilun Wang, of the department of orthopedics at Xiangya Hospital in Changsha, the investigators noted prior research suggests dysbiosis may playing a contributing role to the occurrence, or even development, of various rheumatic diseases. The gut microbiota has an established association with various disease conditions including obesity, growth disorders, metabolic diseases, and mental illness.
“The emerging evidence in the past decades suggests that dysbiosis in gut microbiota and its impact on the balance between pro- and anti-inflammatory immune responses may contribute to the occurrence or development of several rheumatic diseases,” investigators wrote. “Since gut microbiota dysbiosis is potentially modifiable, it has been postulated to be a promising preventive or therapeutic target for rheumatic diseases.”
Wang and colleagues analyzed observational studies evaluating associations between dysbiosis and rheumatic disease via PubMed, Embase and Cochrane Library. They estimated a standardized mean difference (SMD) of α-diversity indices between prevalence of rheumatic disease versus control, while also qualitatively summarizing β-diversity indices and relative abundance of gut microbes.
Their assessment included 92 trials with 11,998 participants; eventually 68 provided data for α-diversity.
The team found consistent α-diversity index decreases for rheumatic diseases overall (SMD, -0.36; 95% CI, -0.63 to -0.09). However, when observing specific diseases, investigators only observed decreases in the following 4 conditions:
- Rheumatoid arthritis (SMD, -0.51; 95% CI, -0.78 to -0.24)
- SLE (SMD, -1.60; 95% CI, -2.54 to -0.66)
- Gout (SMD, -0.64; 95% CI, -1.07 to -0.22)
- Fibromyalgia (SMD, -0.28; 95% CI, -0.44 to -0.11)
Interestingly, investigators observed an associated increase in α-diversity indices with systemic sclerosis (SMD, 1.25; 95% CI, 0.09 - 2.41).
Ankylosing spondylitis and immunoglobulin G4 (IgG4) related diseases were associated with statistically-significant differences in β-diversity.
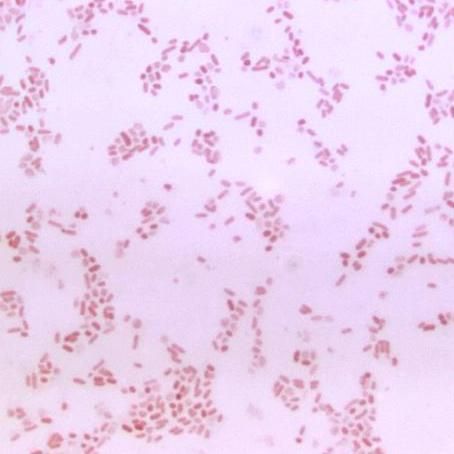
Depletion of Faecalibacterium—an anti-inflammatory butyrate-producing microbe—and enrichment of Streptococcus—a pro-inflammatory microbe—were observed in instances of rheumatoid arthritis, Sjorgen’s syndrome, and SLE. However, whenever the gut microbes merited specificity, investigators observed weaker reproductions, meaning that disease-specific alterations of gut microbes are still uncertain without further research.
Though they caution interpreting the findings—as the observed microbial associations may indicate a shared alteration to multiple rheumatic disease instead a disease-specific biologic difference—the team concluded the observed altered microbes and their metabolites could be used as “general targets for innovative preventive or therapeutic tools for different rheumatic diseases.”
“Finally, little evidence of distinct disease-specific alterations in gut microbes was evident,” they concluded. “This suggests that gut microbes serving as diagnostics for specific rheumatic diseases warrants further investigations.”
The study, “Gut dysbiosis in rheumatic diseases: A systematic review and meta-analysis of 92 observational studies,” was published online in The Lancet Discovery Science.




