Home-Based Exercise Program Improves Quality of Life for Patients With Juvenile Dermatomyositis
“Preliminary evidence has suggested that an exercise training could be effective in improving physical function and quality of life in juvenile dermatomyositis, without exacerbating the disease,” investigators stated.
A 12-week home-based training program was associated with improvements in both overall health and health-related quality of life (HRQL) for patients with juvenile dermatomyositis (JDM) during the COVID-19 pandemic, according to a study published in Pediatric Rheumatology.1
“Preliminary evidence has suggested that an exercise training could be effective in improving physical function and quality of life in JDM, without exacerbating the disease,” investigators stated. “As the social distancing measures due to the pandemic have led to reductions in physical activity levels among healthy individuals and patients with chronic diseases, we speculated that a home-based exercise program could benefit patients with JDM during the outbreak.”
Between July and December 2020, investigators in Brazil developed this prospective, quasi-experimental, mixed methods study to determine the effects of an exercise program for this patient population. The Research Electronic Data Capture (REDCap®) distributed the questionnaires both before and after the program.
Eligible patients were diagnosed with JDM, between the ages of 10 and 19 years, and had received care from the Pediatric Rheumatology Unit of the Children’ and Adolescents’ Institute and the Juvenile Rheumatology Outpatient Clinic, Clinical Hospital, University of Sao Paulo (HC-FMUSP). Patients with chronic kidney disease, chronic pulmonary disease, cardiovascular issues, or undernourishment were excluded.
Participants were required to perform aerobic and bodyweight exercises 3 times a week for 12 weeks. Warm-ups included jumping jacks, skipping, and mobility and flexibility exercises. Bodyweight exercises, such as squats, push-ups, crunches, planks, and lunges, were utilized to work the major muscle groups. Two sessions were unsupervised and 1 was supervised by a trainer. The number of sets, repetitions, and time duration increased every 4 weeks.
Participants were given instructional materials illustrating the exercise program and received a video call prior to the beginning of the training program designed to provide further details and obtain information on each patient’s health status. Adherence was captured via a training log, accounting for both supervised and unsupervised sessions.
The Strengths and Difficulties Questionnaire (SDQ), a behavioral screening tool designed to evaluate mental health disorders, was given to all patients. The questionnaire is divided into 5 sub-scales, including emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems, and prosocial (positive) behavior. Patients and their parents also completed the Pediatric Quality of Life Inventory (PedsQL 4.0), which focused on physical, emotional, and social aspects, and school-related concerns. Sleep was assessed by the Pittsburgh Sleep Quality Index (PSQI), including quality, duration, disturbances, efficiency, and daytime dysfunction. Rheumatic disease was analyzed via the Manual Muscle Test (MMT), Disease Activity Score (DAS), and the Childhood Muscle Assessment Scale (CMAS).
Data was collected at Week 4 and after the program’s completion. Participants were asked what they did or did not like about the training program, how it could be improved, and if they noticed any differences in their health.
A total of 11 patients (91% female) were included in the study. The mean age was 13.5 years, mean Body Mass Index (BMI) was 21.7 ± 6.6 kg/m2, and average time since diagnosis was 7.6 years.
Program adherence was 72.6% (including dropouts) and 80.9% (excluding dropouts). No adverse effects were reported by participants.
Slight improvements were seen in the SDQ Total Difficulties Score and Emotional Problems Score, as well as the PedsQOL School Functioning Score (− 2.4; 95% confidence interval [CI] -5.1; 0.2, p = 0.06; − 1.0; 95%CI -2.2; 0.2, p = 0.09; 11.7; 95%CI -2.5; 25.8, p = 0.09, respectively). However, the remaining domains were unaffected.
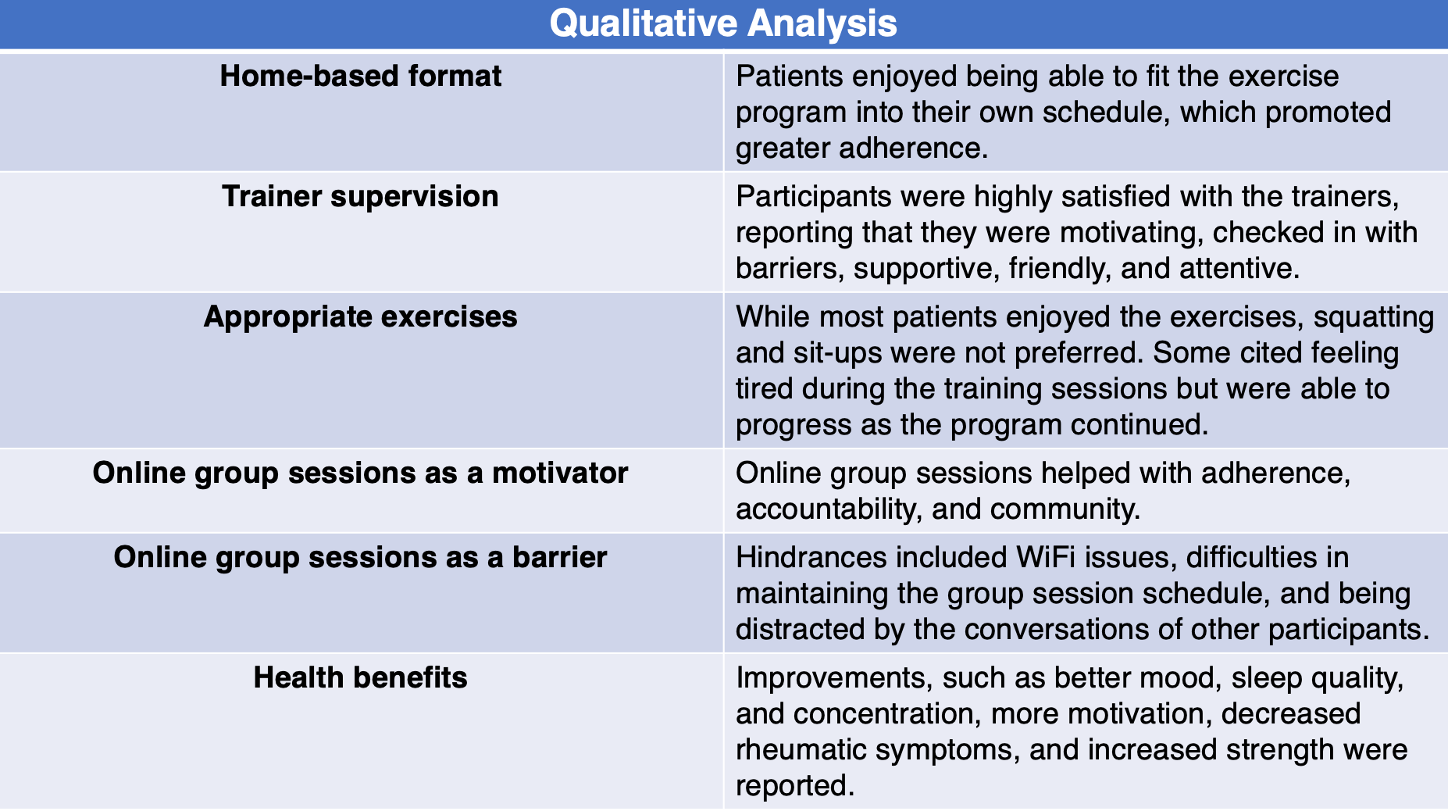
Six themes were determined from patients’ and parents’ comments.
The mixed methods approach and the development of a training program geared towards pediatric patients with rheumatic disease strengthens this study. However, limitations include the small sample size, lack of control group, and the absence of post-intervention assessments and objective outcomes.
“Lessons learned from this trial may help develop cross-culturally adapted, exercise interventions focused on tackling physical inactivity in JDM, especially during these unprecedented times when patients have stayed home to avoid infection complications,” investigators concluded.
Reference:
Astley C, Sieczkowska SM, Marques IG, et al. Home-based exercise program for adolescents with juvenile dermatomyositis quarantined during COVID-19 pandemic: a mixed methods study. Pediatr Rheumatol Online J. 2021;19(1):159. Published 2021 Nov 13. doi:10.1186/s12969-021-00646-7