How to Manage Acute Coronary Syndrome
A 46-year-old man with a history of anxiety and chest pain and a family history of hyperlipidemia drives himself to the emergency department after experiencing non-pleuritic, non-radiating chest pain and dyspnea while playing basketball about 30 minutes earlier.
A 46-year-old man with a history of anxiety and chest pain and a family history of hyperlipidemia drives himself to the emergency department after experiencing non-pleuritic,
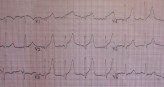
Figure 1. ECG tracing obtained on arrival at emergency department.non-radiating chest pain and dyspnea while playing basketball about 30 minutes earlier. He states he recently had a negative stress test, but this chest tightness feels worse than what he has experienced in the past and is lasting longer.
On physical examination he is hyperventilating at a rate of about 32 breaths/min. Blood pressure is 143/98 mm Hg, pulse, 109; and pulse oximetry is 100% on room air. He is still sweaty but his skin is warm. His lung sounds and heart sounds are both normal except for rate. He has no edema and symmetric pulses in all extremities without delay. The rest of his physical exam is normal.
His ECG is shown in Figure 1, at right (click on images to enlarge).

Figure 2. Tracing of ECG repeated 10 minutes after initial test.
Which of the following should you do next?
A. Give aspirin PO
B. Start lorazepam IV
C. Give nitroglycerine SL
D. Perform serial ECGs
E. Activate the cath lab
ANSWER: All of the above
Discussion
This gentleman certainly appears anxious, but he also has multiple risk factors for coronary disease. A recent negative stress test can be reassuring, but most myocardial infarctions (MIs) are caused by unstable plaques that do not block enough flow to cause a positive stress test, so caution is indicated. Although rare, there are cases of ST elevation MI within a week of a normal stress test.
If a patient is hyperventilating, lorazepam may help him or her feel better, and lowering the respiratory rate may reverse a metabolic alkalosis, which can contribute to narrowing of the coronary arteries. Administering aspirin is almost always wise in a patient with chest pain. Nitroglycerine is an appropriate intervention for chest pain presumed to be cardiac, provided there are no contraindications. Pulse >100 can be considered a contraindication, but his pulse slowed to the 90s soon after his arrival at the ED. Based on history, possible hyperacute T waves, and possible ST elevation in V1, the cath lab was activated, although we were suspicious that the ECG changes might be no more than benign early repolarization. Figure 2, above, shows an ECG tracing obtained 10 minutes after the first.
ECG changes in acute coronary syndrome (ACS) vary. ST-segment elevation, the most ominous finding, is present in about 40% of MIs and is an indication for immediate intervention with fibrinolytics or cardiac catheterization. Dynamic ECG changes or ST-segment depression are also ominous but less so and warrant aggressive medical therapy and eventual catheterization, usually within 24 to 48 hours of presentation. Since the ECG is so important to determining how aggressive therapy should be, it is important to compare the current ECG with an old one if available or obtainable and to repeat the ECG if symptoms are of recent onset or have recently changed because the ECG changes may “evolve” over time.
It is important to be aware of pitfalls in ECG interpretation for ACS. The initial ECG can be normal in about 10% of cases, even during chest pain, and show nonspecific changes in another 5% to 15% of cases. If the clinical presentation is concerning, a single unimpressive ECG should not provide a sense of security. Also remember that unstable angina is diagnosed by the history, since ECGs and serial troponins may not demonstrate any abnormality. This patient was taken to the cardiac cath lab and a 99% occlusion was found in the proximal left anterior descending artery that was opened and stented. For more details on ECG changes in ACS see the Table below.
Table.
ECG in Acute Coronary Syndrome
from Quick Essentials Emergency Medicine pocketbook
Severity:
ST↑ > dynamic â³’s > ST↓ (50% from MI) > LBBB > paced > old MI > deep/peak T > LVH
Get serial ECGs if recent onset or change & old ECG if possible (call PMD or other hospital)
STEMI minutes: tall, peaked or flipped T waves from ischemia
STEMI hours: ST elevation from injury (may last days: reciprocal ST-depression in ≈80%)
STEMI later: Q-waves from infarct (permanent in ≈85%)
ST elevation: 40%, or ST depression: 75%, or old MI: 85%, or NSSTWC: 90%. Normal: 10%
>1 mm except in V2-V3 where it’s >1.5 mm in women, >2 mm in men >40y & 2.5 mm men <40y
Get old ECG to see whether changes are new. If not new, are they chronic or recurrent?
Clinical presentation is important in determining who needs cath lab or lytics
Concave up or subtle ST↑, peak T. ECG normal in ≈10% of ACS, even during the chest pain
Not checking medics ECG &/or old ECG. No repeat ECG done, serial changes missed
Abbreviations: LBBB, left bundle-branch block; LVH, left ventricular hypertrophy.