Hyperkalemia Secondary to Acute Renal Failure
A 35-year-old man presents to the emergency department complaining of syncope. He denies any preceding chest pain, palpitations or trouble breathing, and states he did not injure himself other than a bump on his forehead.
A 35-year-old man presents to the emergency department complaining of syncope. He denies any preceding chest pain, palpitations or trouble breathing, and states he did not injure himself other than a bump on his forehead. On arrival he says he has a mild headache but has not vomited and the headache is improving. He mentions that for the past few days he has had a “pins-and-needles” sensation in both hands and has experienced generalized weakness, but has been able to function. He is otherwise healthy and does not routinely see a doctor.
Physical examination is unremarkable except for a blood pressure measurement of 189/122 mm Hg and a contusion just above his eyebrow. His lungs are clear and he has no cardiac murmur. He also has a normal neurologic exam including short-term memory so a CT of the head is not ordered.
Blood is sent for routine laboratory work up and an ECG is done; the tracing is shown in the Figure.
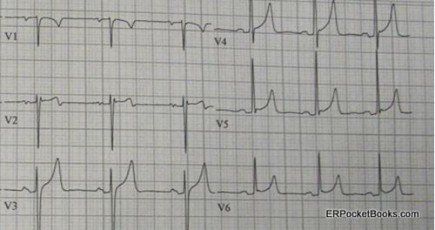
Figure. ECG tracing post syncope
What ECG findings should you look for in a tracing for a patient who has fainted?
What does this ECG suggest?
Answers
In general, in a patient with syncope, the ECG should be checked for abnormal intervals rather than for signs of ischemia. A short PR interval or a long QT interval could be a hint that there has been a recent dysrhythmia. Other conditions to look for that are beyond the scope of this article would be Brugada syndrome or an epsilon wave.
Although this patient’s ECG shows somewhat peaked T waves that could be consistent with benign early repolarization, the differential diagnosis of pronounced or peaked T-waves also includes electrolyte abnormalities, especially hyperkalemia. The patient’s potassium level came back at 8.4 mEq/L without hemolysis. He was in acute renal failure, likely the result of long-standing undiagnosed hypertension.
Discussion
Hyperkalemia is often asymptomatic, but as the potassium level rises it may produce, fatigue, generalized muscle weakness, and paresthesias. The most feared complications of hyperkalemia involve cardiac electrical and rhythm disturbances, usually starting with peaked T waves and prolongation of the PR interval but progressing to bradycardia, a variety of types of heart blocks, and eventually asystole (see Table 1 for additional information).
There are a number of causes of and contributors to hyperkalemia. Usually there is renal insufficiency present of some degree, but a number of other medical conditions and multiple common medications, eg, sulfa antibiotic and ACE inhibitors to name a few, often contribute to this potentially life threatening electrolyte abnormality (see Table 2 for additional details).
Treatment of hyperkalemia can be categorized by mechanism of action. Intravenous calcium acts rapidly and helps to stabilize the cardiac membrane. Insulin + dextrose, albuterol, and sodium bicarbonate all act fairly quickly to shift potassium into cells, temporarily lowering serum levels. Furosemide (Lasix), sodium polystyrene (Kayexylate), and hemodialysis all remove potassium permanently from the body but may take hours to take effect (see chart below for details). Depending on the potassium level and ECG changes, one, more, or all of these medications may be used.
Table 1.
HYPERKALEMIA
from Quick Essentials Emergency Medicine 1-minute Consult pocketbook
Table 2.
Treatment
Lasix
K>7, incr QRS, decr Ca*
cardiac protection
3 amps over 3 min
1-3 min
avoid in digoxin OD
30-60 min
- Calcium: some use if K>6.5 or in rhabdo or tumor lysis (rapid K incr). Insulin: use ≤5units if renal or liver disease.
Click on Image for Details
Table 2.