Improving Pain Management in Juvenile Idiopathic Arthritis Through Decision Support Interventions
Common themes among patients and parents included a need to accurately assess pain and offer non-pharmacological options for pain management.
Results of a recent interview-based analysis demonstrated the need for evidence-based information and communication regarding pain management options to improve pain in patients with juvenile idiopathic arthritis (JIA), according to a study published in Pediatric Rheumatology.1 Investigators believe this could be accomplished by physician training about pain and shared decision making (SDM), as well as using decision support interventions that address these needs.
Most patients with JIA experience some level of pain, and 17% develop chronic pain. This symptom often negatively affects health-related quality of life and activity participation due to difficulties in physical, emotional, social, and school functioning. Further complicating matters, pain in this patient population is regularly under-recognized and communication is not ideal. To effectively manage pain in JIA, a multi-disciplinary strategy, which includes physical, psychological, and pharmacological interventions, is necessary.2
An optimal way to make decisions, especially when there is no perfect treatment option and the choice depends on what families value most, is to engage in SDM,” wrote Karine Toupin-April, PhD, associate professor at the School of Rehabilitation Sciences, Faculty of Health Sciences, University of Ottawa, Canada, and colleagues. “When supported by decision support interventions, SDM can lead to improved knowledge of treatment options, decisions which are consistent with patients’ values, and increased patient participation in decision-making.”
Semi-structured interviews were conducted, either virtually or face-to-face, with young patients with JIA (aged 8 – 18 years), their parents or caregivers, and health care providers (HCPs). Participants were recruited online across Canada and the United States. Interview guides designed to assess decision-making needs were based on the Ottawa Decision Support Framework (ODSF). Investigators audiotaped, transcribed, and analyzed the interviews to identify common themes.
In total, 12 patients (n = 6 children and n = 6 adolescents), 13 parents or caregivers, and 11 HCPs participated in the interviews. Among the pediatric HCPs, 4 were rheumatologists, 3 were physical therapists, 2 were rheumatology nurses, and 2 were occupational therapists. Among patients, 11 were girls and 8 reported inactive disease.
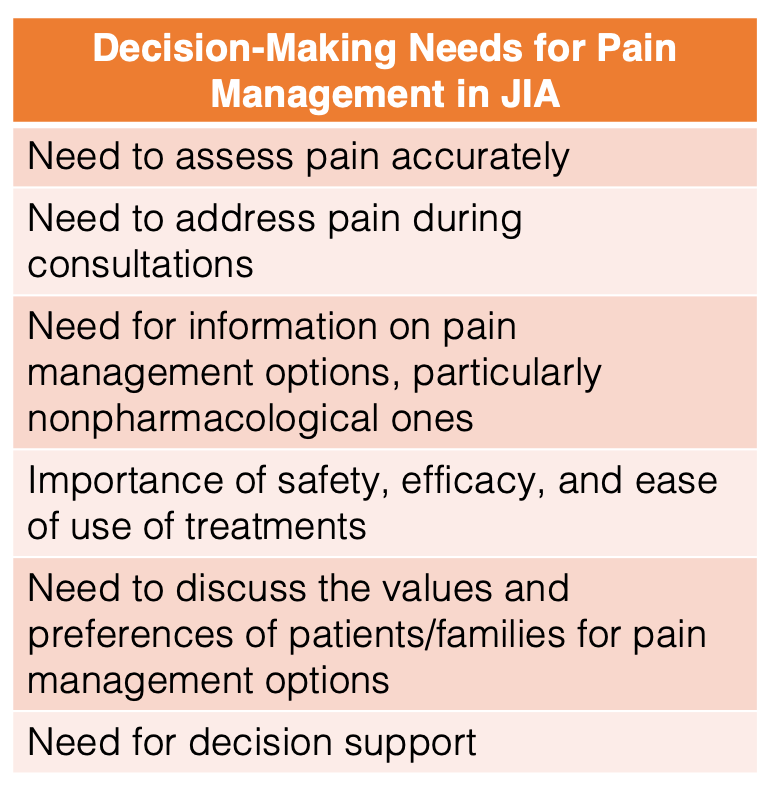
Six themes emerged: 1) the need to assess pain accurately, 2) the need to address pain during consultations, 3) the need for information on pain management options, particularly nonpharmacological ones, 4) the importance of safety, efficacy, and ease of use of treatments, 5) the need to discuss the values and preferences of patients/families for pain management, and 6) the need for decision support. These themes were comparable among patients, parents and caregivers, and HCPs, although importance varied.
Regarding accurate pain assessment, many parents believed it was difficult to evaluate their child’s pain because they were relying on the child’s self-report, which may not always be accurate. Families also mentioned clinic visits generally revolved around disease activity and medications, instead of specifically about pain. Patients and parents expressed a desire to know more about treatment options, although HCPs interviewed stated they were not knowledgeable about nonpharmacological treatment.
Barriers to optimal decision-making included a feeling of pressure to use pain medication and confusion about which drug to choose. Concerning decision support interventions, HCPs stated a tool designed to help describe pain and give information on a variety of treatments may be beneficial. They recommended creating an app or an easily assessable website in addition to routine visits.
Investigators noted generalizability may be limited as most patients were girls, lived in Canada, and had polyarthritis or oligoarthritis. Additionally, they were unable to recruit other relevant HCPs, such as psychologists. However, the psychologists included in the research team will aid in the development of future decision support interventions.
“Work is underway to develop such interventions and implement them into practice to improve pain management in JIA and in turn lead to better health outcomes,” investigators concluded.
References
- Toupin-April K, Gaboury I, Proulx L, et al. "I'd like more options!": Interviews to explore young people and family decision-making needs for pain management in juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2023;21(1):74. Published 2023 Jul 26. doi:10.1186/s12969-023-00849-0
- Weiss JE, Luca NJC, Boneparth A, Stinson J. Assessment and management of pain in juvenile idiopathic arthritis. Pediatr Drugs. 2014. https://doi.org/10.1007/s40272-014-0094-0