Incessant Automatic Focal Atrial Tachycardia
Over-drive suppression of sinus node function by the AT focus occurs in patients with underlying sick sinus syndrome.
An 83-year-old women without known cardiovascular issues presents to the ED after experiencing acute onset palpitations, dyspnea and chest pain while eating dinner.
On physical exam she is alert but looks fatigued. Vitals show a temperature of 98.6, pulse of 170, BP of 85/46, respiratory rate of 27 and pulse ox of 91% on room air. Her physical exam is significant for regular rapid heart sounds without murmurs, bibasilar pulmonary crackles, elevated jugular veins and trace bilateral ankle edema.
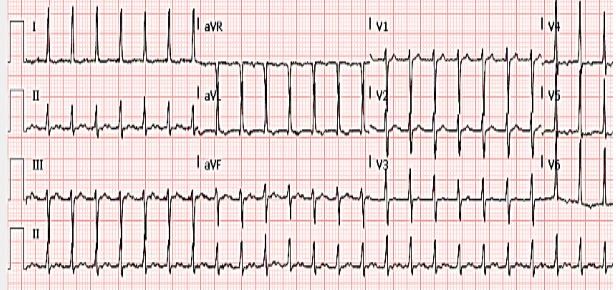
The 12-lead ECG on presentation is shown below:
Question 1: What is the differential diagnosis of this patient’s arrhythmia?
Answer 1.
The ECG shows a regular narrow complex tachycardia with upright P-waves in leads II, III, and avF approximately at the mid-point between QRS complexes. This is therefore a long RP tachycardia (RP interval > PR interval) with a differential including atrial flutter, atrial tachycardia, atypical AVNRT, and orthodromic AVRT. The latter 2 diagnoses involve antegrade conduction over the AV node to the ventricles (QRS complex) with slow retrograde conduction over a slow pathway or an accessory pathway, and would typically manifest negative P-waves in the inferior leads (leads II, III, avF). The P-waves seen in the inferior leads of our ECG are positive, therefore an AV-nodal dependent reentrant arrhythmia is less likely.
Question 2: What diagnostic and potentially therapeutic interventions are now indicated?
Answer 2.
Adenosine administered via bolus infusion may be diagnostic and potentially therapeutic. Temporary AV block induced by adenosine can either unmask the underlying atrial activity of an atrial flutter/tachycardia or convert an AV nodal dependent SVT to sinus rhythm. If adenosine is ineffective then rate control can be attempted with AV nodal blocking agents, unless this is precluded by hypotension at which point DC cardioversion should be performed. In this case, adenosine would break the ongoing rhythm to a long asystolic pause with immediate resumption of the identical SVT.
She remained hypotensive and symptomatic therefore cardioversion was performed, however the SVT persisted, with her ECG now showing:
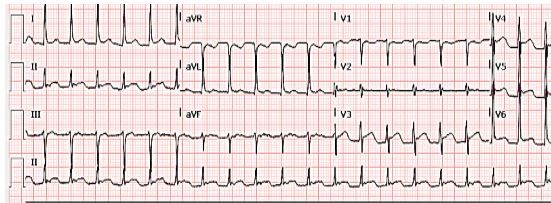
Question 3: What new findings are seen on the ECG and what is now indicated?
For answer and continuation of case, please continue to page 2, below.
Answer 3.
The ECG now shows diffuse ST elevation, most prominent in the inferolateral leads. ST elevation with chest pain should always raise immediate concern for an acute coronary syndrome. Transient ST elevation, however, may occur after direct current cardioversion. Our patient was appropriately at this time transferred for emergent coronary angiography. This showed normal coronary arteries with globally depressed left ventricular systolic function at 40%. The SVT persisted and the patient became progressively hypotensive, tachynpeic and hypoxic requiring intubation and pressor support. Continued attempts to treat the SVT were made with boluses of IV metoprolol, diltiazem and amiodarone.
Following the aforementioned therapy a subsequent EKG was performed:
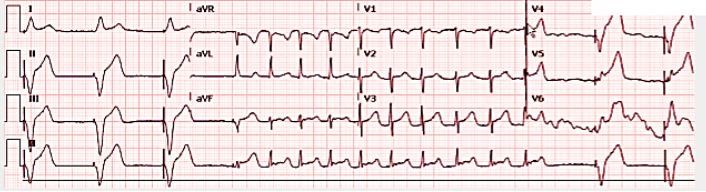
Question 4. What does the ECG now show and what is your next step?
For answer and continuation of case, please continue to page 3, below.
Answer 4.
The ECG demonstrates refractory SVT with long conversion pauses that required placement of a temporary transvenous pacing wire. As the patient has failed cardioversion and medical therapy, and has remained persistently hemodynamically unstable in this rhythm, this is a rare instance where an emergent invasive electrophysiology study (EPS) is indicated. EPS involves advancing mapping electrode catheters via the femoral veins to the endocardial surface of the heart to delineate the exact arrhythmogenic focus, which can then undergo catheter ablation to restore sinus rhythm.
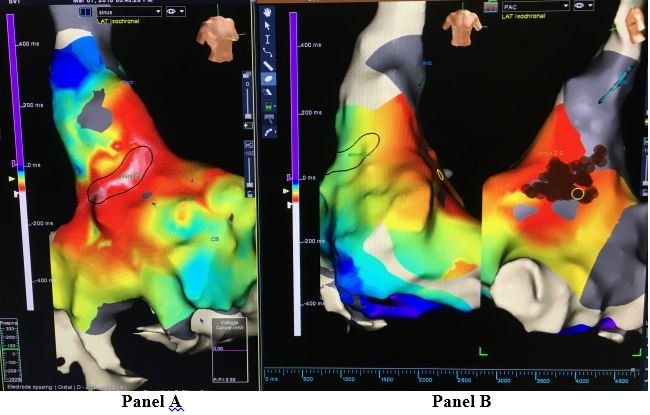
Three-dimension electrical intracardiac anatomic mapping was performed during ongoing arrhythmia and pinpointed earliest activation of the SVT to a superior-anterolateral region for the right atrium (circled white region of interest- panel A of illustration), thus diagnostic of a right atrial focal tachycardia. Radiofrequency ablation at this focus (brown dots- panel B of illustration) terminated the incessant atrial tachycardia to marked sinus bradycardia, requiring atrial pacing support, thereafter with marked improvement in the patient’s hemodynamics.
She ultimately underwent dual chamber pacemaker implantation and has not had recurrent atrial arrhythmias.
Discussion
An automatic atrial tachycardia (AT) may be incessant and cause tachyarrhythmia induced systolic dysfunction leading to hemodynamic compromise. Over-drive suppression of sinus node function by the AT focus occurs in patients with underlying sick sinus syndrome (as with our patient). In these cases, attempts to terminate the AT with cardioversion and/or IV AV nodal blockers may lead to asystolic pauses with resumption of the same tachycardia focus, manifesting as a refractory SVT. Class I and III anti-arrhythmic drugs may be utilized, however they are more effective in suppressing rather than terminating an automatic atrial focus, and can exacerbate underlying sinoatrial and atrioventricular node disease. Refractory SVT, particularly when associated with hemodynamic compromise, warrants cardiac electrophysiology consultation for possible invasive management for diagnosis and therapy.