Measuring the Diameter of the Pancreatic Duct During Secretin Stimulation Is Not a Reliable Test for Pancreatic Insufficiency
A trial designed to find a quick and definitive way to test for exocrine pancreatic insufficiency in cystic fibrosis patients has instead discovered another feasible method that does not work.
A trial designed to find a quick and definitive way to test for exocrine pancreatic insufficiency in cystic fibrosis patients has instead discovered another feasible method that does not work.
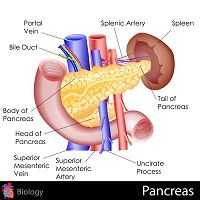
Investigators from Poland enrolled 37 cystic fibrosis patients in the trial and used secretin-enhanced magnetic resonance cholangiopancreatography (SE-MRCP) to compare the pancreatic duct diameters of the 21 pancreatic insufficient patients and the 16 pancreatic sufficient patients.
Images were taken of the head, body and tail of each patient’s pancreatic duct 1, 2, 3, 5 and 10 minutes after initial secretin administration, but only 2 of those 15 sets of images showed any measurable difference between the 2 patient groups.
The diameter of the pancreatic duct, as measured at the head of the pancreas, was slightly larger in pancreatic insufficient patients than in pancreatic sufficient patients at 5 minutes (median, 2.0 mm; interquartile range [IQR], 1.6 mm to 3.0 mm vs. median, 2.0 mm; IQR, 1.0 mm to 2.0 mm; p=0.047) and at 10 minutes (median, 2.0 mm; IQR, 1.4 mm to 2.0 mm vs median, 1.0 mm; IQR, 1.0 mm to 2.0 mm; p=0.040).
Areas under ROC curves for pancreatic insufficient and pancreatic sufficient patients, however, were not significantly different, so they could not be used for patient discrimination. They were 0.693 (95% confidence interval [CI], 0.521-0.866) and 0.698 (95% CI, 0.528-0.868), respectively.
“The measurement of the diameter of the pancreatic duct during secretin stimulation does not
allow for differentiating between pancreatic sufficient and pancreatic insufficient status in cystic fibrosis patients,” the investigators wrote in the Journal of Gastrointestinal and Liver Diseases.
Distinguishing pancreatic sufficient and pancreatic insufficient cystic fibrosis patients as early as possible can improve care for everyone, the investigators noted. Early identification means early treatment with enzyme replacement therapy for pancreatic insufficient patients and early efforts to prevent and detect pancreatitis for pancreatic sufficient patients.
Unfortunately, all of the testing methods that are widely used today suffer from various drawbacks, which led the Polish team to consider the use of SE-MRCP.
“Secretin is a gastrointestinal hormone that is produced by a subclass of duodenal cells in response to acidic pH, which stimulates bicarbonate secretion by the pancreas. It was shown in an animal model that secretin stimulation fails to increase the volume of the pancreatic fluid and to render it more alkaline when cystic-fibrosis-transmembrane-conductance-regulator function is not preserved,” wrote the study authors, who hypothesized that such differences in the response to secretin might make the hormone a tool for distinguishing between pancreatic sufficient and pancreatic insufficient patients.
The new study is not the only effort to use secretin for such a purpose. Researchers reported last year that short endoscopic secretin tests can accurately differentiate cystic fibrosis patients with exocrine pancreatic insufficiency from those who retain exocrine pancreatic function.
The study team gave intravenous secretin to 31 cystic fibrosis patients and 25 healthy controls and, within the next 30 to 45 minutes, used endoscopes to collect duodenal juice. They then analyzed the duodenal juice to determine the concentration of HCO3 and pancreatic enzymes. They also analyzed patient stool to look for fecal elastase.
Both the stool and duodenal juice analyses revealed that 13 of the cystic fibrosis patients maintained exocrine pancreatic sufficiency, while the remaining 18 were not making enough digestive enzymes.
Indeed, the duodenal juice analysis found distinctly differentiated patterns of bicarbonate concentrations and enzyme activities in all 3 types of subject: the cystic fibrosis patients with pancreatic function, the cystic fibrosis patients with pancreatic insufficiency and the healthy volunteers (P < 0.001). The study also found a strong association between severe cystic fibrosis genotype in both alleles and pancreatic insufficient phenotype (P < 0.001).