MS Patients Much More Likely to Have Uveitis, According to Review
An association is logical: nerve and eye tissue develop from the same cells.
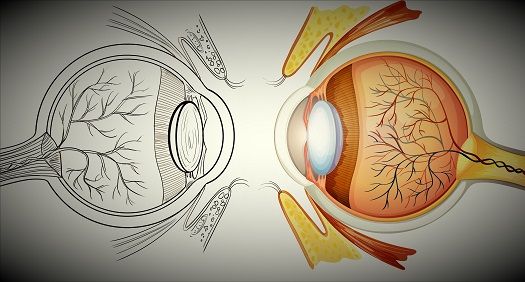
The association between multiple sclerosis (MS) and uveitis has been a matter of debate for decades. Such an association might be expected, because both nerve and eye tissue develop from the same embryonic cells. Moreover, according to a recently published literature review, the largest retrospective studies available indicate that the prevalence of uveitis among MS patients is approximately 1% and the prevalence of MS among uveitis patients is similar. Both prevalences are substantially greater than those found in the general population.
Tine Olsen, MD, and Jette Frederiksen, MD, DMSci, of the Department of Neurology at Rigshospitalet—Glostrup in Glostrup, Denmark, included 35 studies found in the MEDLINE database from 1948 to 2015 in their review. Roughly half of the studies evaluated uveitis patients, half evaluated MS patients, and one study evaluated both MS patients and uveitis patients. Most of the studies were retrospective records reviews.
Several of these studies evaluated 1,000 patients or more. The reviewers categorized these as large studies and noted that they all used contemporary criteria to diagnose MS and uveitis. Specifically, the McDonald criteria were used to diagnose MS, and the Standardization of Uveitis Nomenclature (SUN) criteria were used to diagnose uveitis. The review authors assumed that results from these large studies would provide estimated prevalences closest to the true prevalence.
In five studies of 1,000 or more patients with uveitis, the prevalence of MS ranged from 0.9% to 1.7% (mean, 1%). In contrast, the average prevalence of MS in 13 studies of 1,000 or fewer patients with uveitis was 8.5% (range, 0.7%—30.4%).
In three studies of 1,000 or more MS patients, the prevalence of uveitis ranged from 0.65% to 1.1% (mean, 0.8%). In contrast, the average prevalence of uveitis in 15 studies of 1,000 or fewer MS patients was 12.3% (range, 0.9%—36.7%). However, the review authors noted that this prevalence estimate was driven by several poor-quality studies of fewer than 100 patients.
Regardless of the size of the group studied, none of the studies reviewed found a prevalence of zero. However, the review authors attributed this finding to selection or publication bias. In addition, the review authors found no clear pattern regarding whether MS or uveitis occurred first.
Four of the largest studies explored the relation between MS and uveitis subgroup according to SUN criteria. In two of these studies, intermediate uveitis was the most commonly reported subgroup and had a prevalence of 61% or 80%, depending on the study. Another study found panuveitis in 39% of patients evaluated and intermediate uveitis in 36%.
“More and better research on this topic is needed in the future,” concluded the review authors, who noted that quality of study design is a major obstacle to finding conclusive evidence regarding the true association between MS and uveitis.
The review, “The association between multiple sclerosis and uveitis,” appears in the January-February, 2017, issue of Survey of Ophthalmology.
Related Coverage:
Researchers in Portugal Examine Role of Interleukin-17 in Uveitis
Multiple Sclerosis: Can Massage Therapy Boost Quality of Life?