New Acromegaly Guidelines
The Endocrine Society has issued a clinical practice guideline for the diagnosis and treatment of acromegaly, a rare condition usually caused by a non-cancerous, growth hormone-producing pituitary tumor.
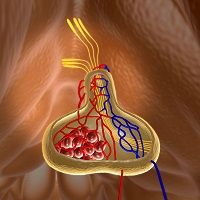
The Endocrine Society has issued a Clinical Practice Guideline for the diagnosis and treatment of acromegaly, a rare condition usually caused by a non-cancerous, growth hormone-producing pituitary tumor. It affects roughly 3 in 1 million people and usually develops in middle age. The Journal of Clinical Endocrinology and Metabolism published the guideline in its November 2014 issue.
Acromegaly results when excess growth hormone causes overproduction of hepatic insulin-like growth factor-1 (IGF-1) to be dumped into the circulation. The overabundance of growth-promoting hormones causes affected individuals to develop exaggerated features. Typical changes include enlarged hands and feet, thickened in the lips, coarsened facial features, protruding forehead and jaw, and widened spacing in the teeth. Acromegaly also increases risk for diabetes, hypertension, heart disease, and sleep apnea.
This new guideline recommends surgery to remove the pituitary gland as the first intervention for most patients. Surgery lowers growth hormone levels immediately and the disease recurs in only 2% to 8% of patients.
If acromegaly symptoms persist after surgery, the guideline recommends medical therapy with somatostatin analogs, pegvisomant, or dopamine agonists. Some patients may require radiation therapy if tumor tissue remains after surgery or in cases where medication is ineffective or intolerable.
Other recommendations from the guideline include:
- Clinicians should order IGF-1 levels in people who have facial features or large extremities associated with acromegaly.
- Random growth hormone measurements are insufficient to diagnose the condition.
- Clinicians need to monitor patients with acromegaly for hypopituitarism.
- Every acromegaly patient’s treatment plan needs to be individualized based on presenting symptoms, pathology, and response to intervention.