Older Patients With RA More Likely to be Undermedicated
“There are no tailored age-specific treatment guidelines, and older adults are less likely to receive aggressive therapy for reasons of polypharmacy and multimorbidity,” investigators stated.
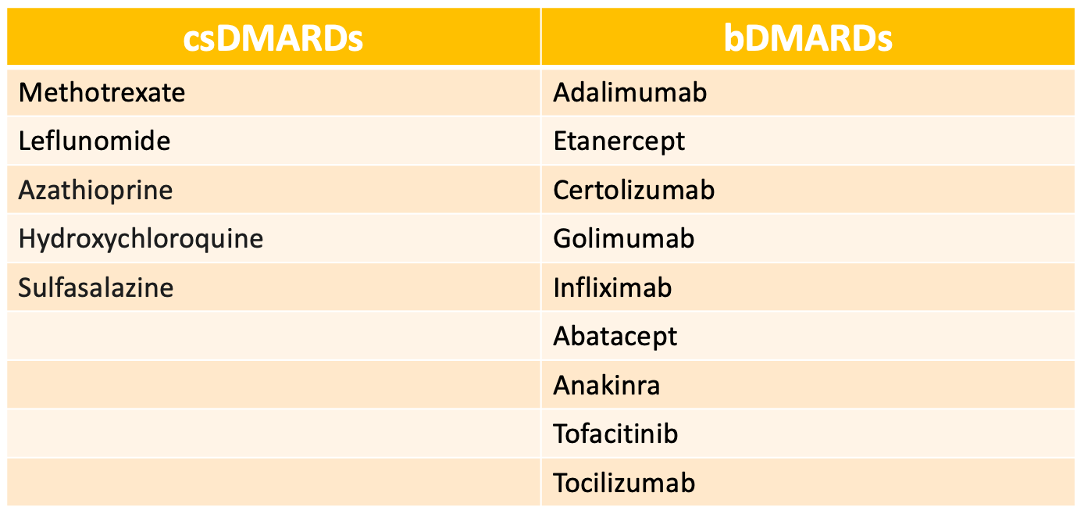
The percentage of older patients with rheumatoid arthritis (RA) receiving disease-modifying antirheumatic drugs (DMARDs), including biologic DMARDs (bDMARDs), remains low despite the recent American College of Rheumatology (ACR) guideline updates which encourage aggressive treatment, according to a study published in Open Rhuematology.1
“There are no tailored age-specific treatment guidelines, and older adults are less likely to receive aggressive therapy for reasons of polypharmacy and multimorbidity,” investigators stated. “This raises concerns for quality of care as a growing population of older adults are living with RA owing to increased life expectancy, along with advancement in understanding and treatment of rheumatic diseases.”
Older adults, defined as aged 65 years or older, were analyzed using national sample office visits. Patients included were seen by either rheumatologists or primary care physicians (PCPs) with information taken from the 2005-2016 National Ambulatory Medical Care Survey (NAMCS). Independent variables collected included demographics, specific diagnosis, medications, provider specialty, and the reason for visit. Polypharmacy was defined as a categorical variable based on the number of non-DMARd medications: 3 or fewer, 3 to 5, or 5 or more. DMARD usage, along with patterns and trends, were determined using multivariable analyses and descriptive statistics. The descriptive analyses evaluated visits and prescriptions of DMARDs through the 12-year study period and categorized them by provider specialty. Multivariable logistic regression models adjusted for age, sex, race and ethnicity, multimorbidity, and non-DMARD polypharmacy.
In total, investigators found 518 observations which represented 7,873,246 office visits from older adults with RA, with 74% being seen by a rheumatologist. Most patients were women (72%) and 85% were White. Approximately half of patients received a DMARD from a rheumatologist (56%) and 30% were prescribed a DMARD from their PCP. While investigators saw in increase in RA-related visits in rheumatology clinics throughout the 12-year period, more patients initially saw a PCP for new condition evaluation (26%) when compared with a rheumatologist (7%).
Among patients receiving DMARDs, 20% of rheumatologists prescribed 2 or more DMARDs, compared with only 6% of PCP visits.
No statistical differences in trends were seen among rheumatologists and PCPs for any DMARD (P = 0.259) or conventional synthetic DMARD (csDMARDs) (P = 0.658). However, bDMARDs were more common among rheumatologists when compared with PCPs (P = 0.004).
While ACR guidelines recommend methotrexate as the first line DMARD therapy, a bDMARD was prescribed 5 times more frequently at rheumatologist visits when compared with PCP visits.
The study was limited due to the complex survey-based observational nature of the analyses. Investigators analyzed the visits associated with RA, not specific patients with RA, and individual cases were not followed over the 12-year period. Further, confirmed diagnosis, medication data, and dosage information could not be validated against prescription dates. Other variables, such as income, education, and disease activity, were not included in the study. However, the NAMCS provides unbiased estimates and allowed investigators to study a large group of visits over an extended period.
“With predicted shortages in the rheumatology workforce and maldistribution of rheumatology providers, PCPs may play an increasingly important role in caring for older adults with RA,” investigators concluded. “Further research is needed to understand to optimize appropriate use of DMARDs in older patients with RA.”
Reference:
Lee J, Chang CH, Yung R, Bynum JPW. Provider Specialty and the Use of Disease-Modifying Antirheumatic Drugs for Rheumatoid Arthritis Among Older Adults in the 2005-2016 National Ambulatory Medical Care Survey. ACR Open Rheumatol. 2022;4(4):332-337. doi:10.1002/acr2.11406