Article
Biomarkers Aid in Diagnosis, Prognosis of Early Multiple Sclerosis
Author(s):
Serum levels of interleukin-7 and C-X-C motif chemokine ligand 10 appeared to provide the most accurate means of identifying large differences in disease risk.
No specific biochemical markers have been available to confirm the diagnosis of multiple sclerosis (MS) — until recently.
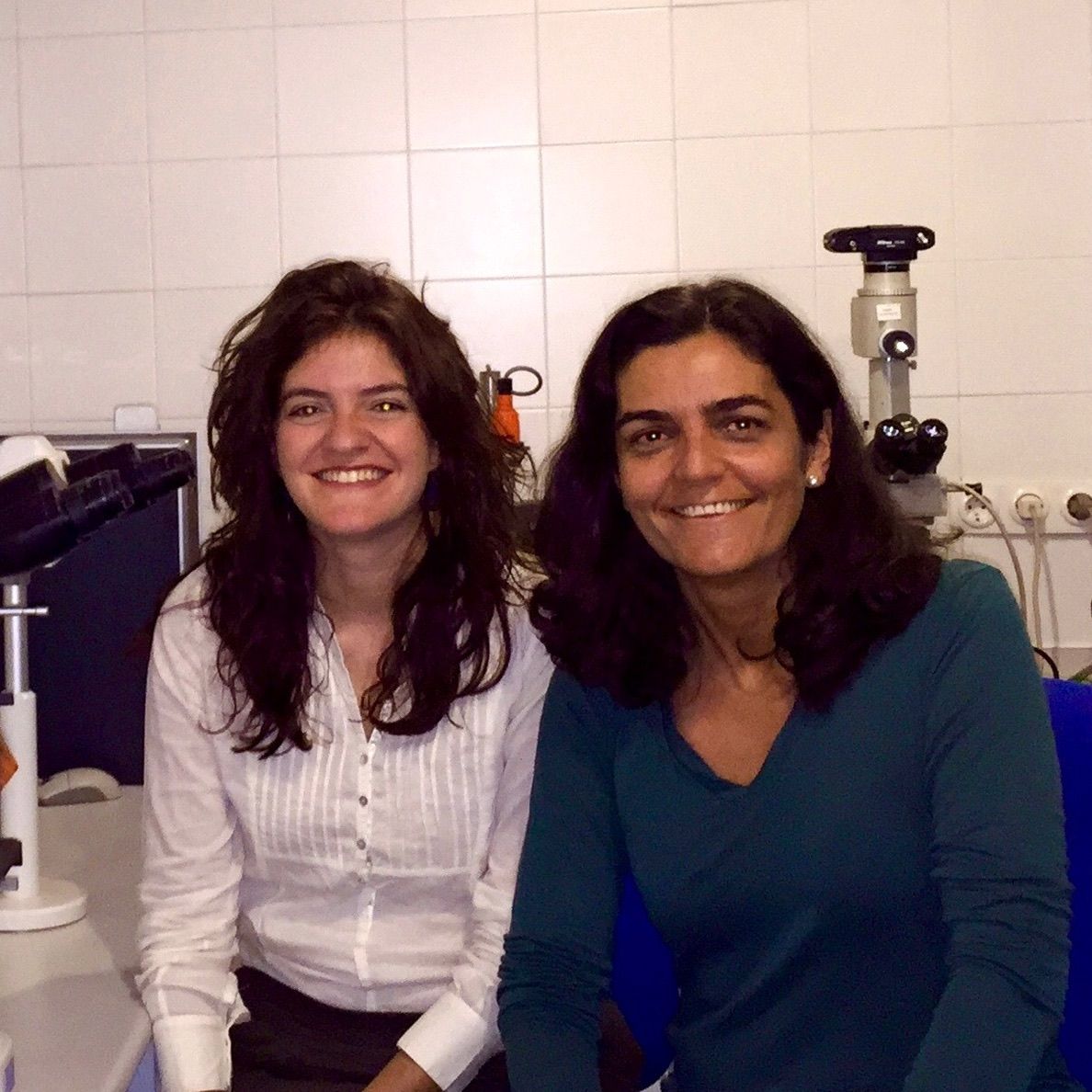
A Spanish and French research team developed a decision-tree based on results of analysis of biomarkers in the serum and cerebrospinal fluid (CSF) of MS patients. Lidia Fernandez-Paredes, MD (left), and Silvia Sanchez-Ramon, MD (right), both in the department of clinical immunology at Hospital Clinico San Carlos in Madrid, Spain, co-led the research team.
This lack of biomarkers often resulted in a delay in MS diagnosis and treatment while clinicians waited for a relapse to occur or for results of sequential neuroimaging studies to confirm the presence of disseminated lesions in the central nervous system. This study was conducted to provide clinicians with a means of diagnosing MS by using specific biomarkers.
In a previous, cross-sectional study in 2 independent cohorts of MS patients, the team used biologically plausible pathways to identify a panel of 12 biomarkers that might enable investigators to discriminate between the 2 main forms of MS at disease onset — relapsing-remitting MS (RRMS) and primary progressive MS (PPMS). An ability to discriminate between the 2 forms could enable clinicians to make a more specific diagnosis and provide more appropriate treatment sooner, which could delay the disease from becoming irreversibly disabling.
In the current study, the team determined which biomarkers in this panel could be most useful in diagnosing MS in the early phases of the disease as well as in predicting its course. To do this, they collected serum and CSF samples from 89 patients who were recently diagnosed with MS, 97 patients with other neurological diseases (59 non-inflammatory and 38 inflammatory), and 46 age-matched, healthy controls.
After analyzing levels of biomarkers in the samples, the team concluded that serum levels of interleukin-7 (IL-7) and C-X-C motif chemokine ligand 10 (CXCL10) appeared to provide the most accurate means of identifying large differences in disease risk. A serum IL-7 level <141 pg/mL identified patients with MS at onset (odds ratio (OR), 6.5; P < 0.001), and those who also had a CXCL10 level <570 pg/mL were at greatest risk of having the primary progressive form of MS (OR, 22; P = 0.01).
“We started this work years ago in close collaboration with Matthew Albert at the Pasteur Institute in Paris,” Sanchez-Ramon told MD Magazine. “This work is the continuation. Validating these markers at the beginning of clinical manifestations could be especially useful for making therapeutic decisions.”
“Once our validation is confirmed by other groups, our decision-tree will provide a practical clinical tool for identifying patients at risk of the progressive form of MS in its very early stages,” she added.
In addition to important findings regarding serum biomarkers, the study team also unexpectedly found a substantially lower level of biomarkers of inflammation and tissue regeneration in the CSF of MS patients than in that of patients with other neurological diseases. The team interpreted this finding as an indication that a defect in the intrinsic immune response contributes to the onset of MS.
A report on the study was published in the August 2017 issue of Clinical Immunology.





