Pulmonologists Favor Antifibrotic Treatment Immediately After IPF Diagnosis
Results from an online, self-administered survey showed a mostly consistent and unified response in pulmonologist treatment responses.
Results from an online, self-administered survey showed a mostly consistent and unified response in pulmonologist treatment responses for idiopathic pulmonary fibrosis (IPF).
Findings from the study, titled “Physician Characteristics Associated with Treatment Initiation Patterns in Idiopathic Pulmonary Fibrosis: Results from an Online, Self-Administered Survey,” were presented at the American Thoracic Society (ATC) 2018 International Conference on May 21, 2018, in San Diego, California in. The survey was designed to evaluate the influencing factors in idiopathic pulmonary fibrosis (IPF) treatments of pulmonologists, in an attempt to pinpoint physician-specific factors that contribute to treatment tactics.
The survey targeted 169 pulmonologists from the Pulmonary Fibrosis Foundation and an included additional responses from an external database of physicians recorded between April 10 and May 17, 2017. Inclusion criteria for the study was dependent on whether the pulmonologist spent > 20% of his or her time in direct patient care and had ≥ 5 patients with IPF receiving antifibrotic therapy.
Questions pertaining to timing and reasoning for the initiation of antifibrotic therapy post-IPF diagnosis; attitudes toward adopting a “watch-and-wait” approach; and the decision-making process for beginning antifibrotic therapy were answered by survey participants. The willingness to consider beginning antifibrotic therapy treatment immediately after an IPF diagnosis categorized the survey responses. Categorizations included “yes, all the time/most of the time” vs “only some of the time/no, usually not.”
According to the results, initiating antifibrotic therapy immediately after IPF diagnosis “all or most of the time was considered by most participants (81.7%, n=139), while initiating treatment “only some of the time” or “usually not at all” was considered by 18.3% (n=31) participants.
Additionally, the likelihood that pulmonologists worked in a private practice (26.1% vs 16.1%), had a greater mean percent of patients currently receiving antifibrotic therapy (60.8% vs 30.5%), and were more likely to make the decision to initiate treatment themselves (31.2% vs 16.1%) was greater in pulmonologists who considered initiating treatment immediately, all, or most of the time. (This data is correlative to pulmonologists who thought of initiating treatment only some of the time or not at all.)
The most common reasons for initiating antifibrotic therapy immediately after IPF diagnosis were results of pulmonary function tests (87.5%), severity of symptoms (79.2%), patient request to start therapy (73.8%), and high-resolution computed tomography findings (72.6%) in both groups of pulmonologists. In addition, utilizing a “watch-and-wait” approach for 32.7% of newly diagnosed patients with IPF was reported by pulmonologists (on average). Patient preference (86.3%), absence of symptoms (79.7%), and minimal abnormalities on pulmonary function tests (72.5%) were main reasons for the “watch-and-wait” method when opted for by pulmonologists.
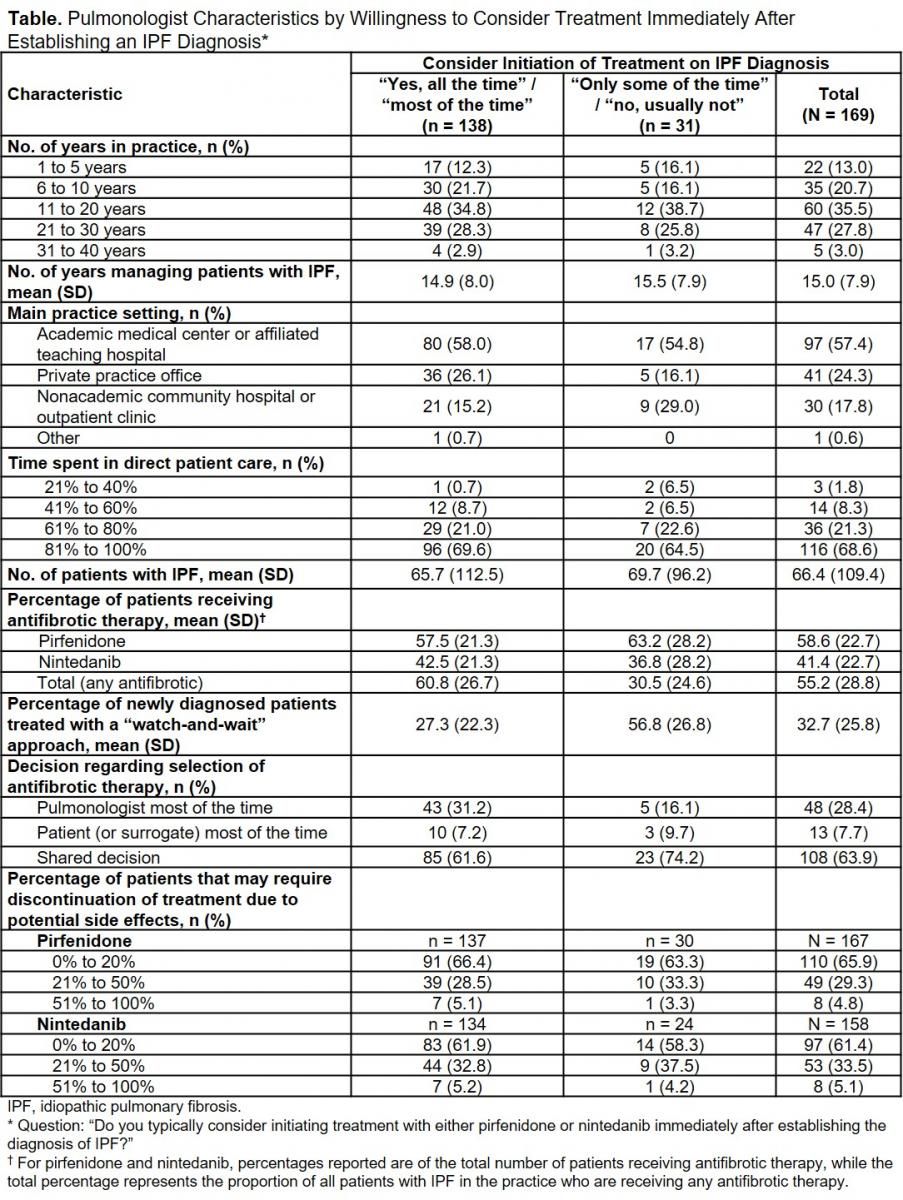
Chart: LaCamera P, et al. Physician Characteristics Associated with Treatment Initiation Patterns in Idiopathic Pulmonary Fibrosis: Results from an Online, Self-Administered Survey. American Thoracic Society 2018 Annual Conference. http://www.abstractsonline.com/pp8/#!/4499/presentation/15317
Based off of the survey results, the study authors concluded that a majority of pulmonologists consider initiating antifibrotic treatment immediately after establishing an IPF diagnosis all or most of the time. However, practice setting, percent of patients receiving IPF therapy, and the decision-making relationships between patients and physicians were identified criteria in distinguishing treatment immediately after diagnosis in contrast to the “watch-and-wait” method.
For more from the rare disease community, subscribe to Rare Disease Report’s e-newsletter.