Researchers Test 5G-Based Technology for Diabetic Retinopathy Care
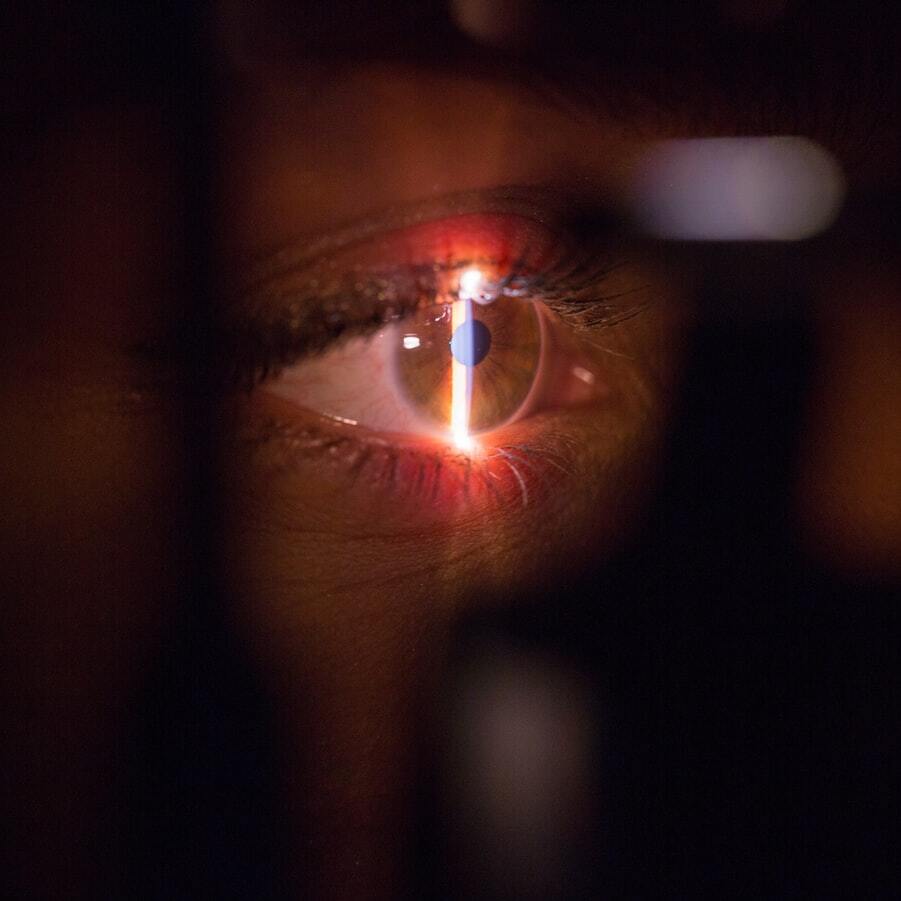
Retinal laser photocoagulation may be performed by a specialist from a distance using telemedicine platforms.
Fifth-generation (5G) technologies hold promise for teleophthalmic practices, particularly for diabetic retinopathy, suggests a new study from China.
“The use of 5G technology to communicate directly with physicians and to share medical records through an online platform has the potential to improve the quality of telemedicine-based DR treatment while engendering trust and enhancing patient-physician relationships,” the investigators wrote.
“The development of laser photocoagulation instruments and new telecommunication platforms have highlighted the promise of therapeutic telemedicine as a means of treating DR."
As such, in order to assess the feasibility of 5G real-time telemedicine-mediated laser photocoagulation as treatment for diabetic retinopathy, the investigative team, led by Huan Chen, MD, of Peking Union Medical College Hospital, performed a double-site, nonrandomized, prospective study involving patients with proliferative or severe nonproliferative DR.
The Promise of 5G
At study outset, Chen and colleagues enrolled a total of 6 patients and 9 eyes.
The team used a teleopthalmology platform that included a laser system for navigated retinal photocoagulation, a TeamViewer platform allowing for remote computer control, videoconference software for consultations, and 5G networks for high-speed transmission.
Prior to intervention initiation, a retina specialist received all patient medical records transmitted through the platform. The specialist then reviewed the data before using the platform’s teleconferencing capabilities to discuss the disease and treatment plans with both the patient and their local ophthalmologists.
Patients were informed of the benefits and risks of 5G-mediated retinal laser photocoagulation, and, following consent, each patient underwent the online-navigated photocoagulation operation.
“The retinal specialist in Beijing remotely controlled the laser device in Huzhou using a computer connected to the platform for remote computer control,” Chen and colleagues explained.
“The operation interface and real-time fundus video, as well as a simultaneous live video from 2 cameras (with one providing a panoramic view of the laser treatment room and another providing close-up shots of the digital laser device monitor) were transmitted from Huzhou to the retinal specialist in Beijing via videoconferencing.”
The specialist proceeded to plan individual therapeutic approaches for each patient by using his finger to define laser areas and caution zones on a color fundus photograph. The laser system then performed photocoagulation based on his input.
Following the operation, Chen’s team assessed eye prognosis as well as real-time laser therapy transmission speed.
Results
Overall, 6 were treated via panretinal photocoagulation alone, 1 eye had focal/grid photocoagulation, and 2 eyes underwent both panretinal photocoagulation and focal/grid photocoagulation.
The team reported that the retinal telephotocoagulation operation was performed on all eyes without any noticeable delay during treatment; even more, all treatment plans were transmitted between sites without error.
The average number of panretinal photocoagulation laser spots for each eye in 1 session was 913.
Further, a total of 7 eyes—or 4 patients— experienced no significant changes in visual acuity through the 1-month period.
However, 2 participants (2 eyes) did not have follow-up until 6 months post-operation as a result of the COVID-19 pandemic. They reported a decrease in visual acuity and poor glucose control, and 1 patient underwent cataract surgery at a local hospital.
In one of the patients, persistent neovascularization 1 month following the first teleretinal laser photocoagulation procedure was observed—as a result, they required top-up PRP.
“The novel technologies used in the present study can be leveraged to educate local ophthalmologists regarding the retinal laser photocoagulation procedure, in addition to improving patient access to services and lowering associated healthcare costs,” Chen and colleagues wrote.
“Using imaging devices and high-speed network transmission to visualize lesions in real time can enable less experienced ophthalmologists to learn the retinal laser photocoagulation approach in an intuitive manner during the telemedicine process, in contrast to traditional telemedicine.”
They indicated that future studies will need to compare approaches between retinal telephotocoagulation and the current standard of care in terms of visual acuity and safety outcomes.
The study, “Application of 5G Technology to Conduct Real-Time Teleretinal Laser Photocoagulation for the Treatment of Diabetic Retinopathy,” was published online in JAMA Ophthalmology.