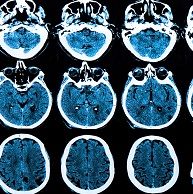
Spinal Cord Imaging Helps Diagnose and Follow MS, But Challenges Remain
Up to 90 percent of patients with multiple sclerosis have spinal cord pathology.
If you ask a patient with progressive multiple sclerosis to define her condition, she may say that she because of multiple sclerosis she has lost her independence, can’t work, and is getting worse.
A radiologist would see:
- Progressive atrophy, expanding lesions
- Reduced MTR, NAA, fractional anisotropy
The neurologist would say:
- Accumulation of disability
- Gradual over time
And a pathologist would believe:
- Axonal pathology
- Oligodendrocyte pathology
At least half of all 2.3 million patients with multiple sclerosis (MS) in the world have the primary-progressive form of the disease (PPMS), but there is no FDA-approved treatment for PPMS. Nearly 10 percent of patients are diagnosed with PPMS upon onset, which is the main determinant of disability. Most MS patients begin with a relapsing form, and then develop PPMS.
Omar Khan, MD, chair and professor of neurology at Wayne State University School of Medicine in Detroit, Michigan, talked about the benefits and challenges of spinal cord MRI during a presentation at the 2015 Annual Meeting of the Consortium of Multiple Sclerosis Centers in Indianapolis, Indiana.
Khan said that primary care physicians can help prevent disease progression by referring patients with potential MS symptoms to a neurologist earlier. Relapsing patients have symptoms that come and go.
Diagnosis should include a neurological history and exam, results from brain and spinal cord magnetic resonance imaging (MRI), and studies such as evoked potentials and spinal fluid testing. He believes that leptomeningeal inflammation may play a significant role in spinal cord pathology of PPMS.
“Seventy to 90 percent of MS patients have spinal cord pathology,” Khan said. Doctors are beginning to appreciate this more and more, particularly in the context of the progressive phenotype. SCA-SC appears to be a robust measure of cord atrophy and has good correlation with disease progression.
Doctors have been imaging spinal cords for years and in fact, Khan talked about one doctor in the audience who was doing this back in 1996 in London. Today, Khan said that spinal cord imaging techniques such as MTR may be useful in linking pathology to imaging markers.
But what are some challenges?
The spinal cord is very small. “The spinal cord is about the size of two-finger widths wide, whether you are an NFL 240-pound linebacker or five-foot 100-pound ballerina. It is very normalized,” Kahn said.
When a patient has any kind of metal in their body in the area to be scanned, the artifacts may limit the usefulness of MRI.
And if a patient breathes too deeply, the radiologist will get blurry images to read. Ultra-high-field magnets that are 7 Tesla or higher provide faster imaging, which help compensate for patient movement and provide a better signal-to-noise ratio.
Claustrophobic patients may require open MRI, although conventional MRI produces clearer images.
Some diseases mimic others. So referring physicians may want to ask for a neuro-radiologist for image interpretation.
The Consortium of Multiple Sclerosis Centers updated its MRI protocol this year. It can be found on the CMSC website homepage at www.mscare.org. The American College of Radiology also offers MRI guidelines on its site at www.acr.org.