Article
Sprifermin Improves Cartilage Thickness, but Clinical Benefit Uncertain
Intra-articular administration of sprifermin statistically increases total femorotibial joint cartilage thickness in individuals with symptomatic radiographic knee osteoarthritis, but the clinical importance and duration of the effect are uncertain, say researchers writing recently in JAMA.
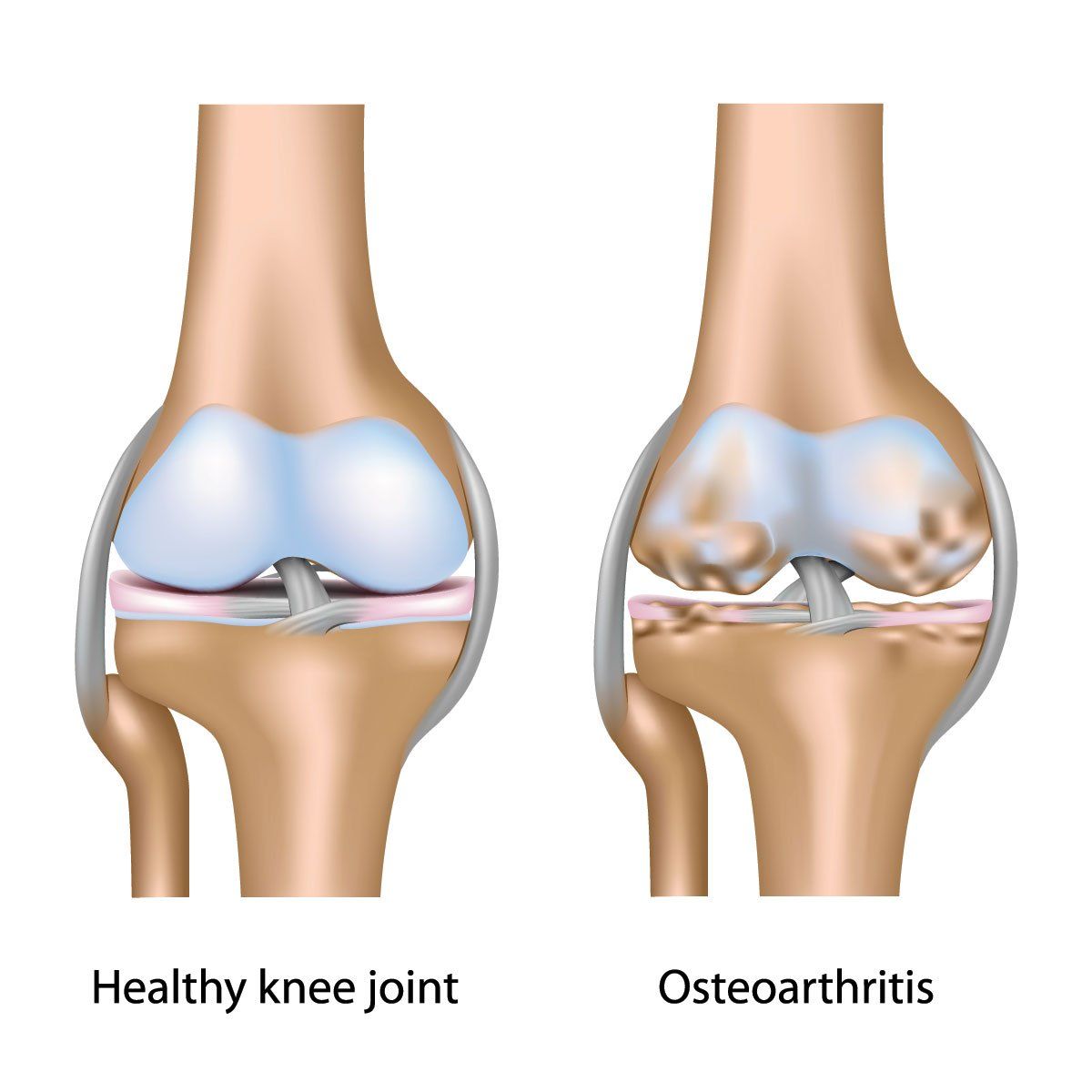
Osteoarthritis (©AlilaMedicalMediaShutterstock.com)
Intra-articular administration of sprifermin statistically increases total femorotibial joint cartilage thickness in individuals with symptomatic radiographic knee osteoarthritis, but the clinical importance and duration of the effect are uncertain, say researchers writing recently in JAMA.
Symptomatic knee osteoarthritis is associated with physical disability, reduced quality of life, and increased mortality in older adults. Current treatments primarily target symptoms, since there are no disease-modifying osteoarthritis drugs approved in the United States or Europe. Sprifermin, a recombinant human fibroblast growth factor (FGF)-18, is under investigation as a potential anabolic intra-articular disease-modifying drug.
Led by Marc C. Hochberg, M.D., MPH, of the University of Maryland, Baltimore, the phase 2 FGF-18 Osteoarthritis Randomized Trial with Administration of Repeated Doses (FORWARD) was a 5-year multicenter randomized clinical trial. The 549 participants were aged 40 to 85 years with symptomatic, radiographic knee osteoarthritis and Kellgren-Lawrence grade 2 or 3.
They were randomized to one of five groups: Intra-articular injections of 100μg sprifermin given every 6 months or every 12 months, 30μg sprifermin every 6 months or every 12 months, or placebo every 6 months. Each treatment consisted of weekly injections over 3 weeks. A total of 474 patients completed two-year followup.
For the primary endpoint, change in total femorotibial joint cartilage thickness measured by quantitative magnetic resonance imaging at two years, statistically significant, dose-dependent increases were seen with sprifermin versus placebo (P < .001 for both treatment effect and dose-response).
By group, the significant increases in joint cartilage thickness from baseline occurred in those given 100μg sprifermin every 6 months and every 12 months (0.03mm and 0.02mm, respectively), while cartilage thickness declined by 0.02mm in the placebo group.
No significant changes from baseline occurred with 30μg sprifermin given every 6 or 12 months (0mm and -0.01mm, respectively). Statistically significant dose-dependent effects in joint space width were seen in the lateral compartment (P = .004 for treatment effect; P < .001 for dose response) for both 100μg sprifermin regimens (0.19mm for every 6 and 12 months) but not in the 30μg groups. The measure dropped significantly in the placebo group (-0.07mm). There were no significant changes in joint space width in the medial compartment.
No statistically significant differences from placebo in any of the dosage groups were seen on the 11-point Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain scale. Scores improved from baseline in all five treatment groups, with no differences compared to placebo in WOMAC subscales for pain, function, or stiffness. Moreover, pain medication use was similar in the sprifermin groups compared with placebo.
“It is possible that using intraarticular saline injections as a control may act as an active placebo, masking symptomatic improvements associated with sprifermin in this study,” the authors suggest.
Arthralgia was the most frequently-reported adverse event reported in all of the treatment groups, ranging from 36% of the group receiving 30μg of sprifermin every 12 months to 45% with 100μg every 12 months. There were no serious adverse events considered to be were considered related to study treatment.
“Analysis of a more select group of participants, who have baseline characteristics associated with rapid structural and symptomatic progression of knee osteoarthritis, may indicate symptom differences vs placebo and should be investigated in future studies,” Hochberg and colleagues conclude.
REFERENCE
Hochberg MC, Guermazi A, Guehring H, Aydemir A, Wax S, Fleuranceau-Morel P, Reinstrup Bihlet A, Byrjalsen I, Ragnar Andersen J, Eckstein F. Effect of Intra-Articular Sprifermin vs Placebo on Femorotibial Joint Cartilage Thickness in Patients With Osteoarthritis: The FORWARD Randomized Clinical Trial. JAMA. 2019 Oct 8;322(14):1360-1370. doi: 10.1001/jama.2019.14735.




