Strategies Are Developing to Boost HIV PrEP Initiation
Stigma, and a lack of communication and awareness all inhibit HIV PrEP uptake, but digital health and new forms of PrEP could boost users.
There had been more 200,000 pre-exposure prophylaxis (PrEP) initiations in North America from 2016-2020, according to data from the AIDS Vaccine Advocacy Coalition (AVAC) earlier this year. While the US is highly contributory to the gradually increasing rate of HIV-risk persons gaining access to PrEP annually, it’s not enough to consider the work accomplished on a national scale.
There are millions of untreated people that could benefit from its use, and the drivers of PrEP underutilization are multifactorial. Despite its proven benefits over the last decade, PrEP is plagued by provider challenges, limited understanding of the market for eligible patients, and prospective PrEP users’ lack of awareness of the prophylaxis therapy.
The challenge of adhering to daily oral PrEP can also pose challenges for its indicated population. Homelessness, injection drug use, and poverty are all factors that limit use. Additional demographic factors, like race, gender, and sexuality, have also been associated with challenges to PrEP uptake. For example, despite their disproportionately high HIV incidence rate, Hispanic and Latino adults were the least likely to be referred for PrEP, per a Centers for Disease Control and Prevention (CDC) study this year.

PrEP disparities are also widened by marketing tactics. Although heterosexuality accounts for the identified sexuality of 23% of all new HIV diagnoses annually, HIV and AIDS are still commonly perceived to only occur among men who have sex with men (MSM), and they are the most likely to be prescribed PrEP. Lingering homophobia creates an intensely negative stigma around HIV that discourages many at-risk persons from seeking PrEP.
Because HIV is a sexually transmitted infection, many at-risk young women forgo PrEP out of fear their family, partner, or community will view them as promiscuous. HIV is the world’s leading cause of death in women 15-49 years of age, but proportionally very few women are taking PrEP.
All these disparities in PrEP uptake and coverage have the potential to be remedied with long-lasting injectable PrEP. Cabotegravir, VIIV Healthcare’s PrEP injectable, could receive Food and Drug Administration (FDA )approval as early as January 2022.
Dawn K. Smith, MD, MS, MPH, medical officer for the CDC noted in a statement that the FDA has set a PDUFA target date of January 24, 2022 for the new cabotegravir indictation. “(The_ CDC added a section about cabotegravir to the latest version of pre-exposure prophylaxis guidelines…so that providers can begin prescribing this new long-acting injectable without delay if and when it is approved,” Smith said.
If approved, cabotegravir would be the first long-acting PrEP therapy available, meaning populations unable or unwilling to adhere to a daily PrEP regimen would have an infrequent, discreet option for HIV prevention.
Suzan Walters, PhD, research assistant professor in the NYU School of Global Public Health, affiliated investigator at the Center for Drug Use and HIV/HCV Research, and faculty affiliate at the Center for Opioid Epidemiology and Policy, studies injection drug use and societal inequities in biomedical intervention, such as PrEP.
Walters told Contagion® that she believes it important “to offer different modalities for all drugs as people have different lives and preferences…All communities stand to benefit from injectable PrEP.”
“I do want to take a moment to express how structural conditions, such as housing and poverty create challenges not only for PrEP but for health in general,” Walters continued. “People who use drugs who also experience housing insecurity often have challenges keeping their property, which could include PrEP, and thus injectable PrEP could mitigate this issue. There have been cases of stollen medications and as such having an option to take PrEP without the obligation to carry it around stands to benefit drug using populations, and likely many other populations.”
Walters added that drug-using populations at high HIV risk have shown capability to adhere to the demands of a daily PrEP pill, but nonetheless have expressed preference in a once-monthly injection option. For the homeless HIV-risk population, the new cabotegravir indication could have the potential to mitigate “structural burdens” associated with homelessness.
“The simple fact of having a choice in how one receives PrEP has the potential to increase uptake,” Walters said. “Choosing the best option for one’s body and lifestyle gives a patient autonomy over their healthcare journey, increasing PrEP uptake and adherence."
That said, there’s a tendency for widening treatment disparities and distribution inequities in instances when health care technological advances are reached. “We have seen this with PrEP in general, with a widening gap in uptake between white communities and communities of color,” Walters explained.
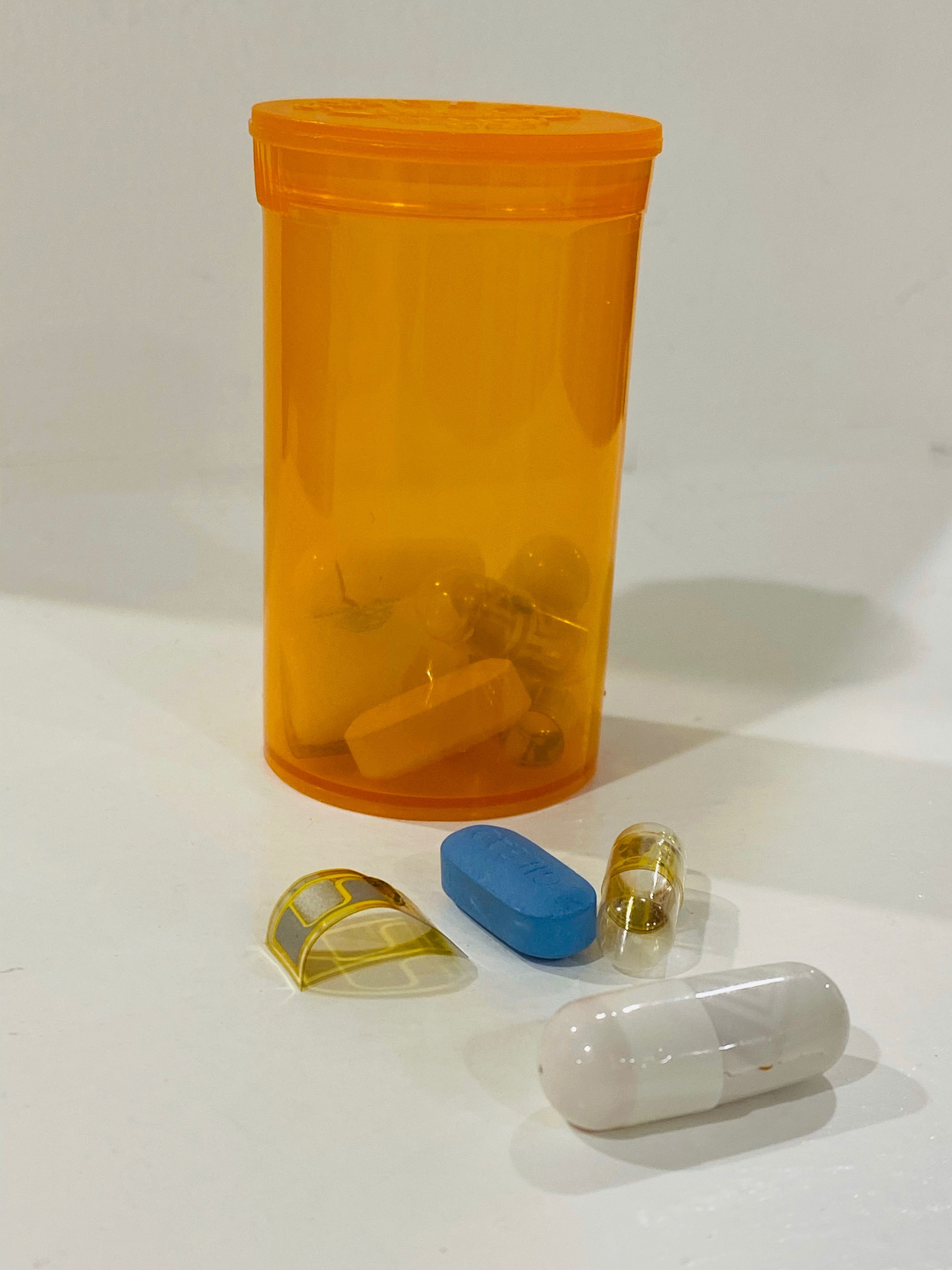
Peter Chai, MD, MMS, of the Department of Emergency Medicine and Medical Toxicology at Brigham and Women’s Hospital, Assistant Professor at Harvard Medical School, and Adjunct Faculty at The Fenway Institute, understands stigma runs deep. He was involved in the development of a digital pill for the use of studying PrEP and ART adherence. He knows PrEP can be recognized as the little blue pill, and they have been able to mask PrEP’s appearance to enable more privacy to users.
“There is this stigma of seeing the blue pill, and we can cover it and change the color to hide the fact people are on it,” Chai said. “We are very aware of stigma and stigma is a huge barrier to adherence.” This is just 1 nuanced approach to help users avoid the stigma associated with the therapy.
Jonathan Hill-Rorie, MPH, project director for our Adolescent Medicine Trials Network for HIV/AIDS Interventions, Fenway Institute, believes part of the low number of PrEP users has to do with who is getting PrEP messaging. “I think what goes on with PrEP marketing and what has gone on for the last few years has been this hyper focus on cisgender men who have sex with men (MSM) as opposed to other high-risk communities such as trans people, women who are engaging in high-risk sex,” Hill-Rorie, said. “The marketing and the way we talk about PrEP is one of the issues.”
Hill-Rorie said in addition to limited marketing, there are structural barriers including insurance challenges; general distrust of the medical community by certain communities; and the ability to obtain medications. Another element of PrEP underutilization is choice. Whereas, younger people may be less inclined to take it, older people may be more open to doing so based on their experience.
The younger generation of HIV-risk persons may not have been shaped by the historically high HIV/AIDS mortality rate and burdens observed in the early decades of the epidemic, before the advent of antiretroviral therapy (ART), Hill-Rorie explained. He pointed out that the younger generation understands the benefits of PrEP, but may not have had the same connotations associated with HIV or the benefit of time to digest the significance of taking this medication.
“Older folks in the gay community who really sing the praises of PrEP understand the importance of a medication that can prevent HIV especially given that many were around in the initial epidemic and saw lots of friends die,” Hill-Rorie explained.
PrEP Provider Bias
Even PrEP providers are not insusceptible to the stigma surrounding HIV and PrEP. A recent study found that PrEP doctors’ racial stereotypes about Black women not being able or willing to adhere to a PrEP regimen prevented them from providing PrEP to this at-risk demographic.
Similarly, PrEP providers are more hesitant to prescribe PrEP to injection drug users than to other at-risk groups,. The stigma surrounding drug use is very prevalent in health care and is likely part of the reason why only 1-2% of injection drug users take PrEP.
Some clinicians have also expressed concerned that prescribing PrEP to certain populations may enable them to forgo other safety measures, such as using condoms.
The CDC updated its PrEP guidelines this year, stipulating that doctors should talk to all sexually active adults about HIV PrEP, and prescribe it to any patient who asks for it. Walters emphasized the importance of doctors talking to their patients about PrEP, as increasing PrEP uptake is not possible without first increasing PrEP awareness.
“We need to scale up PrEP care across the PrEP care continuum, beginning with awareness for injectable PrEP to be a success,” Walters said.
Researchers have pointed out that it is not the role of PrEP providers to make judgements of who is “deserving” of PrEP, but rather prescribe HIV PrEP based upon available data of the groups with the highest risk of HIV infection.
“The populations I work with are often structurally disadvantaged and face severe forms of stigma, including stigma in health care,” Walters said. “In order for us to increase PrEP and in turn lower HIV incidence we really need to tackle some of the root causes of inequities. This means we need to address housing, poverty, and stigmas, including racism. It will be very hard to address HIV if we do not address the real causes of health disparities.”
Getting More Providers Prescribing PrEP
HIV treatment specialist Gary Spinner, DMSc, PA, MPH, AAHIVS, is the Medical Director of the HIV/AIDS Program at Southwest Community Health Center and leads his center's initiatives on PrEP. He says he would like to see more primary care providers engaging in conversations with patients about their sexual health, which could lead to greater utilization of PrEP.
Spinner pointed out there might be just 1 PrEP prescriber in many medical settings, which means there are lost opportunities to engage many more patients in counseling on this form of HIV prevention. At Spinner’s center, they not only have a PrEP navigator to help with these conversations and get the right candidates into the treatment funnel, but there are providers across specialties at Southwest who are having PrEP conversations with patients and prescribing the therapy as well.
“One of the things I’ve really focused on is offering numerous trainings to my colleagues in primary care in my community health center, so I am no longer the sole prescriber of PrEP,” Spinner said.
How Technology Can Help People with Sexual Health
Technology is frequently used in health care field to garner greater insights about people’s behaviors, and HIV is no exception. In PrEP, investigators are looking to gain greater access to patient data, use it to serve as daily reminders, and aid in better patient outcomes.
The Fenway Institute has been deeply involved in digital health studies and just finished recruiting for its COMPARE study, which explores the use of 2 apps to help young people better understand and manage their sexual health including possibly looking at PrEP utilization. Hill-Rorie said they are using both the My Choices and Links apps, to study people’s behaviors and that are looking at trying to help prevent HIV in young people.
In the former, the app uses quizzes and information about PrEP to educate users, and helps them make informed decisions about it. The latter app uses what Hill-Rorie said is “sex positivity” to think more critically about decisions around sex.“Those 2 apps are going to be compared to see which aspects of the 2 apps were most useful in increasing HIV and STI testing and getting folks on PrEP,” Hill-Rorie, explained.
The idea is to take the positive aspects of each of the apps and combine it into one app, so it has all these components, “to help them take ownership of the sexual health.”
Hill-Rorie said there are a multitude of ways technology can help with PrEP utilization, including who are local PrEP providers in the area, and sending daily reminders to people’s phones to make sure they are taking their medication. And although the common thought is that younger people would are more comfortable with telemedicine, Hill-Rorie said the younger generations still like to have in-person discussions.
“That is a very prevalent idea, particularly because we are in this digital era now where Gen Z is on Tick Tock, and millennials are deeply invested in Instagram and Facebook, and everything is marketed via social media,” Hill-Rorie said. “I think the knee-jerk thing is to do everything via social media and digitally. I think there are digital benefits to doing that…but I think young people are just as impacted by face-to-face and in-person interactions as well because there is a level of trust that is built when you are able to engage people one-on-one, in groups, or going into a community space and being able to talk through [things].”
Overall, clinicians have 2 PrEP challenges: the first is to get people on it; the second is to get people to stay on it.
Fenway has its LifeSteps study, which is geared towards helping people who have recently started taking PrEP, stay on their regimen. “This is an intervention where a nurse sits with a young person to talk with them about issues they are having with adhering to their medication and giving them general knowledge around sexual health,” Hill-Rorie said.
This counseling includes information on STIs and risk assessments. Over the course of 4 weeks of counseling, they can come up with strategies and solutions to overcome any barriers with PrEP adherence.
Digital Pills
Chai has been involved in developing ingestible electronic sensor systems to understand medication adherence in the context of substance use and HIV treatment and prevention. His work in developing ingestible sensors, or “digital pills,”are being used to study behavioral interventions to measure, reinforce, and provide tools for PrEP and ART adherence. His work has been funded by the National Institutes of Health (NIH), and the sensor technology has been featured as a top innovation of 2021 by Popular Science.
The digital pill is made up of a few components including a standard gel capsule, the PrEP pill itself, a radio frequency emitting device, and a wearable reader and smartphone app that lets users check their adherence. The pill and the radio frequency emitting device are placed inside the capsule. Study participants ingest the digital pill, and once it enters the stomach, acids dissolve the gel capsule. The radio frequency emitter, which is approximately the size of a sesame seed, sends a signal about 3 feet off the body that’s picked up by the wearable reader. Chai said the reader is a lanyard device that is approximately the size of an ID badge.
“There is a radio frequency transmission, and we code it to drug, time, and date. The reader sends that information to the smartphone app. Patients can look at the app and see their adherence data on demand,” Chai explained. “On the clinical side, we can also see that data and it allows us to have this interface where we can push reminders or interventions specifically around PrEP and ART adherence around individuals who are using the system.”
One of the digital pill studies Chai is working on with Fenway is the Tech PrEP Study. This specific study focuses on MSM and use substances. This study is a survey being done through use of a popular dating app. “We are trying to find out what people think about digital pills—the [aspects of them] that are really interesting to them, but also some of the pieces that are scary to them.”
In addition, Chai said is looking to learn more about substance use and PrEP adherence. “We know from a lot of clinical trial work that most of the difficulty around PrEP adherence can come when people are using different substances because it clearly changes routines, can make people forgetful, and things like that,” Chai said. “This digital pill can reinforce the behavior of taking your PrEP despite the fact you might be taking substances.”
Another study Chai and Fenway are starting up is the PrEPsteps study. Fenway is currently recruiting people for it and their aim is to utilize an investigational smartphone-based intervention and digitized emtricitabine 200 mg and tenofovir disoproxil fumarate 300 mg (Truvada) digital pill daily for 3 months to help improve adherence to PrEP.
“What we really want to know is how people are taking PrEP day-to-day,” Chai, said. “The digital pill is this marker that helps us annotate during somebody’s daily activities when they took their PrEP.”
Conclusions
Up to 99% effective with regular use, PrEP has significantly decreased HIV infections worldwide. But uptake and adherence remain low, especially among marginalized groups already at increased risk of contracting HIV, despite PrEP now becoming available under most healthcare plans.
Unfortunately, the deeply negative stigma surrounding HIV and HIV preventative measures augment the spread. PrEP providers and all doctors should educate their patients that HIV is not something shameful; it is an infectious disease that anyone can and does contract, but disparate incidence rates are due to societal inequities and are not intrinsic to the disease itself.
PrEP prescribers should undergo bias training to be made aware of any stereotypes they may have internalized that impede them from fairly prescribing HIV PrEP. Additionally, they should become familiar with the social factors that make certain populations more likely to develop HIV infection, and work to end disparate HIV incidence in marginalized communities.
Increased national and global HIV efforts help mitigate HIV incidence, but as one of the most effective tools available, the importance of utilizing PrEP cannot be overstated. Technological advances continue to boost the ease and accessibility of PrEP, but eradicating HIV will not be possible without first eradicating HIV stigma.
For anyone who lives in the Boston area who might be interested in participating in the PrEPsteps study, Fenway can be contacted through email at prepsteps@fenwayhealth.org or by phone at (617) 927-6266.