Universal Decolonization Significantly Lowers MRSA Rates in ICU Patients
The largest study to date on reducing rates of methicillin-resistant Staphylococcus aureus (MRSA) infections in ICU patients found that bloodstream infections in these patients can be reduced by more than 40 percent through universal decolonization practices.
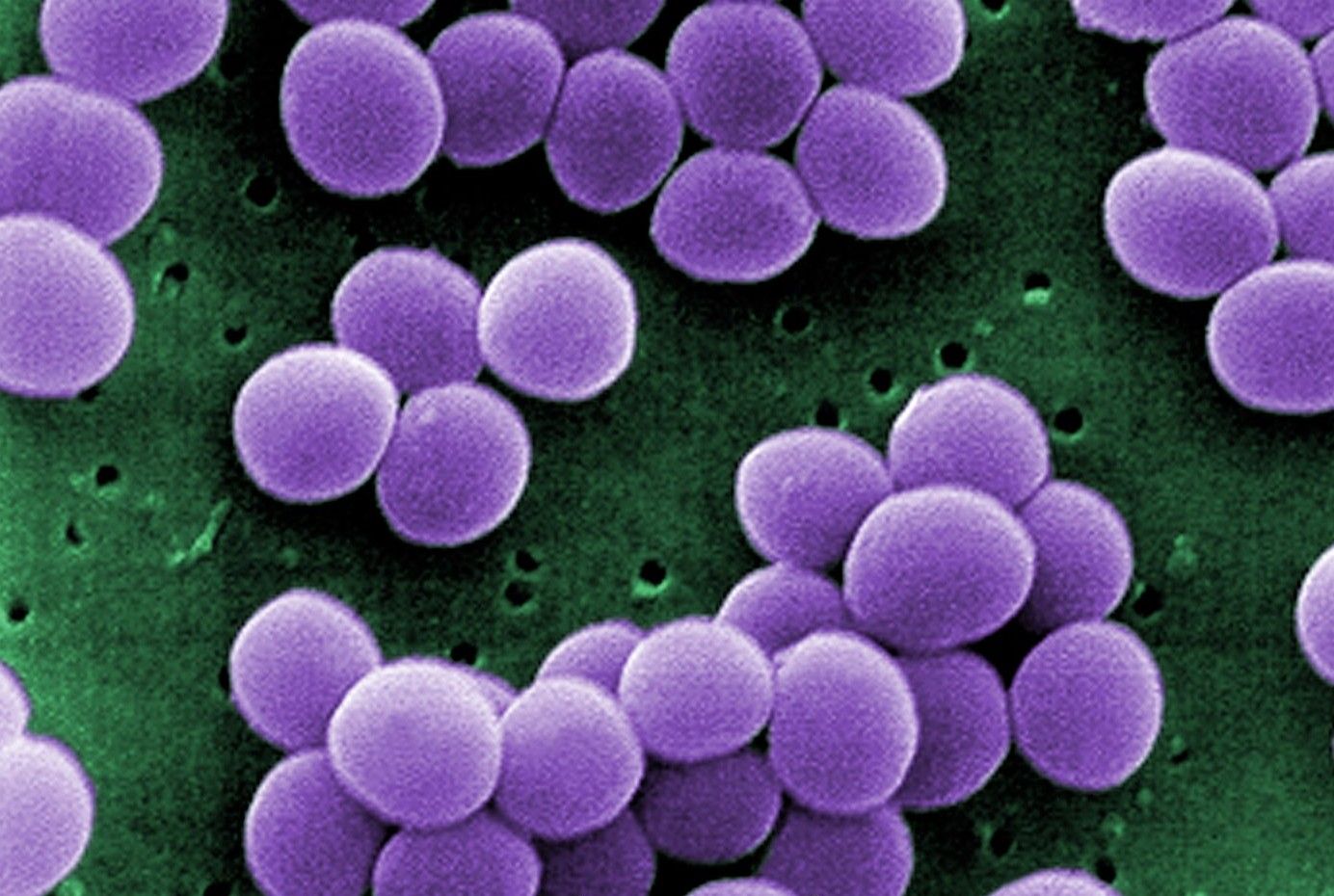
The largest study to date on reducing rates of methicillin-resistant Staphylococcus aureus (MRSA) infections in ICU patients found that bloodstream infections in these patients can be reduced by more than 40 percent through universal decolonization practices.
The study, REDUCE MRSA, compared universal decolonization practices to targeted decolonization or screening and isolation to reduce rates of MRSA clinical isolates and bloodstream infections from any pathogen.
The study was carried out by the US Centers for Disease Control and Prevention (CDC) and the Hospital Corporation of America (HCA) in more than 43 US hospitals and included more than 74,000 ICU patients from 2009 through 2011. Proportional hazards models were used to assess differences in infection reductions across the study groups, with clustering according to hospital.
In the intervention versus baselines periods, hazard ratios for bloodstream infection with any pathogen in the 3 groups were 0.99, 0.78, and 0.56, respectively, (P<0.001 for test of all groups being equal). Universal decolonization resulted in a significantly greater reduction in the rate of all bloodstream infections than either targeted decolonization or screening and isolation. One bloodstream infection was prevented per 54 patients who underwent decolonization.
Lead study author Susan Huang, MD, MPH, an associate professor at the University of California Irvine School of Medicine and Medical Director of Epidemiology and Infection Prevention at UC Irvine Health, said the results helped answer a long-standing debate about whether doctors should tailor their efforts to prevent infection to specific pathogens, such as MRSA, or identify a high-risk patient group and give them all special treatment to prevent infection.
“The universal decolonization strategy was the most effective and the easiest to implement,” she said. “It eliminates the need for screening ICU patients for MRSA.”
The study was published in June 13, 2013, edition of The New England Journal of Medicine.