Article
Update on Joint Replacement: Benefits and Concerns
Recent years have witnessed tremendous advances in the field of orthopedic surgery, particularly in total joint arthroplasty.
ABSTRACT:There have been tremendous advances in total joint arthroplasty (TJA) in recent years, and the number of TJA procedures has increased significantly. As the number of patients living longer with knee replacements continues to increase, the complications also will increase. Important but controversial is prophylaxis for venous thromboembolism prevention after TJA. The advent of metal-on-metal bearings for total hip arthroplasty promised decreased wear, but many recent reports of problems have prompted the issuance of guidelines for managing patients with these implants. One factor thought to be decreasing the length of hospital stay after TJA is the use of less invasive surgical approaches. The success of highly cross-linked polyethylene has been a game-changer in hip replacement by increasing the longevity and functionality of the replacement.
Recent years have witnessed tremendous advances in the field of orthopedic surgery, particularly in total joint arthroplasty (TJA). Along with total knee arthroplasty (TKA) and total hip arthroplasty (THA)-both known to impart functional benefit to patients-arthroplasty of other joints (eg, shoulder, elbow, and ankle) have become common procedures.
Because of the immense success of TJA and an increase in patients with degenerative joint disease, the number of procedures has risen rapidly over the past decade. With more and more patients in need of well-functioning joint replacement, the field is rising to the challenge of providing long-lasting, functional, pain-free replacements.
Marked improvements in techniques for anesthesia and delivery of surgical care associated with TJA have accounted for notable reductions in postoperative complications and better outcomes. Recent advances in pain management have made procedures less painful and have enhanced postoperative recovery and rehabilitation. Although joint replacement technology is not without challenges, the quality and functionality of arthroplasty components continue to improve.
In this article, we provide an update on recent developments in TJA procedures. We describe the recent increase in the number of procedures performed, the new modalities and changes in recommendations for prophylaxis of venous thromboembolism (VTE) after TJA, the issue of using metal-on-metal (MOM) bearings, concerns in perioperative management, and the use of highly cross-linked polyethylene (HCLPE) for the bearing surface.
INCREASED USE OF TKA
The number of TJA procedures, particularly TKA procedures, has increased significantly in recent years. Total knee replacements performed in the United States doubled from 1999 to 2008.1,2 More than 600,000 TKAs were performed in 2008.
Insights into this trend were provided by a study of patients with TJA presented at the 2012 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS).3 Through the use of a computer simulation model combined with US census data, the authors found that more than 4.5 million persons currently are living with at least 1 TKA, translating to 4.5% of the US population older than 50 years. The prevalence continues to increase with aging of the population-it is likely that 10% of persons older than 80 years will have at least 1 knee replacement.
The reason for increased utilization of TKA is not entirely clear. It has been shown that factors beyond the aging of the patient population and increases in Medicare patients and societal obesity are contributing.2 One important factor is thought to be expanding of indications to younger patients.
As the number of patients living longer with knee replacements continues to increase, the complications associated with knee replacements also will increase. Specifically, revision TKA surgery and periprosthetic fracture are expected to be more common in the practices of orthopedic surgeons who manage patients who have undergone total knee replacement.
The increase in utilization of TKA comes at a time when the need for knee replacement in patients with rheumatoid arthritis (RA) continues to decrease. The advent of tumor necrosis factor α inhibitors and similar medications has substantially decreased the progression and severity of RA and, hence, the need for TKA in patients with RA.
PROPHYLAXIS FOR VTE PREVENTION
Important but controversial is prophylaxis for VTE prevention after TJA. Surgeons are faced with the task of balancing the risks of VTE with the morbidity associated with administration of prophylaxis, such as postoperative bleeding. Identification of patients at risk for VTE versus those at risk for bleeding continues to present a challenge.
In an effort to guide orthopedic surgeons in this difficult task, the American College of Chest Physicians (ACCP) and the AAOS have proposed guidelines for prevention of VTE after TJA. Both organizations updated their guidelines recently.4,5
The previous guidelines differed in their recommendations-the ACCP endorsed more aggressive anticoagulation-but the updated guidelines from the organizations are more in concordance. Recognizing the significant morbidity associated with postoperative hematoma formation and wound drainage and the need for subsequent surgery, both organizations now endorse the use of less aggressive therapies, such as aspirin and mechanical prophylaxis, in preventing VTE.4,5
The pharmaceutical companies continue to search for better agents to be used for VTE prevention. Although numerous drugs have been launched recently, including factor Xa inhibitors that can be administered orally and do not require monitoring, the increased effectiveness of these agents appears to come at the cost of an increased risk of bleeding.
Different Strategies
A majority of orthopedic surgeons continue to use traditional VTE prophylactic methods, which fall into 1 of 3 general categories: warfarin, injectable anticoagulants (including fractionated heparin), and aspirin in combination with mechanical methods. The recent literature has suggested that the incidences of clot formation associated with these methods are similar.
One study evaluated 94,000 patients who underwent elective TKA over a 2-year period.6 Patients were managed with 1 of the 3 protocols according to surgeon preference. Sophisticated statistical analysis was used to adjust for bias.
The risk of a thromboembolic event was lower in the patients who were managed with aspirin or an injectable agent. The risk of complications associated with surgery did not differ among the groups. The patients who were managed with aspirin had fewer medical comorbidities before the surgery and had a shorter length of stay postoperatively, suggesting that differences in perioperative care contributed to the patients' outcomes. Another study that evaluated 27,000 patients who underwent THA found no difference in the incidence of pulmonary embolism or death among patients managed with aspirin, injectable anticoagulants, or warfarin.7
In our practice, we have adopted a multimodal strategy that involves preoperative risk assessment to identify patients who are at increased risk for VTE or bleeding. We use regional anesthesia to facilitate pain control and allow for early mobilization. For patients who are not at increased risk for VTE, we have resorted to the use of aspirin and mechanical prophylaxis.
MOM BEARINGS IN THA
These bearings have attracted much attention recently. What was once touted as a solution to the problem of wear in hip replacements has turned into a frequent billboard ad for plaintiffs’ attorneys. The advent of MOM bearings promised decreased wear and allowed for the use of larger femoral head sizes, possibly leading to a decrease in the incidence of instability. Recently, however, many reports of problems have prompted both the British Hip Society (BHS) and the FDA to issue guidelines for managing patients with these implants.8,9
FIGURE
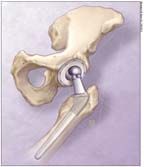
The number of total joint arthroplasty procedures for patients with degenerative joint disease has risen rapidly over the past decade.
The most publicized MOM issue was the recall of the Articular Surface Replacement (ASR) resurfacing prosthesis (DePuy Orthopaedics, Warsaw, Indiana) in August 2010. Early results for patients who had the ASR implanted showed failure rates in excess of 10%, prompting the recall. More recent midterm follow-up has found that the failure rate continues to increase. A UK study that used Kaplan-Meier analysis showed a failure rate of 48.8% at 6 years.10
Generation of Metal Debris
Most of the early failures appear to be related to generating metal debris, and it has been established that MOM articulation does so. The recent literature has shown that a cup abduction angle greater than 40° could pathologically generate more of this debris.11
Increased metal debris translates to elevated metal ion levels in patients, which have been shown to be associated with aseptic lymphocytic vasculitis-associated lesion and adverse local tissue response (pseudotumor).12 Both soft tissue responses are associated with increased pain and revision.
Even with these more sophisticated modes of failure, the most common reason for revision after MOM THA continues to be aseptic loosening. The increased incidence of this problem with MOM hips is not completely understood. In addition, an alarming incidence of failures resulting from pain seems to be unexplained.
More Difficult Workup and Management
The implications of the ASR recall and associated litigation make the workup and management of patients with MOM hips all the more difficult. Recently, the BHS recommended extended follow-up for patients with MOM hip replacement,8 including yearly evaluations for all patients.
In our practice, patients with MOM hips who are asymptomatic and have cup abduction angles of less than 40° are monitored on an every-other-year basis. Workup of a patient with a painful MOM hip begins with a traditional approach. The patient's C-reactive protein level and erythrocyte sedimentation rate are obtained to evaluate for the possibility of infection; elevation of either value prompts an aspiration. If the workup for infection is negative, serum cobalt and chromium tests are ordered; elevation of either value beyond 7 parts per billion is concerning. We recently began to use metal artifact reduction sequence MRI for further evaluation of patients for pseudotumor and other soft tissue lesions. Our threshold for revision in the setting of any positive finding is low.
PERIOPERATIVE MANAGEMENT
As medical costs continue to rise, hospitals and care providers have an incentive to decrease the inpatient length of stay after surgery. The length of hospital stay after joint replacement has decreased considerably in recent years. Most facilities have a length of stay between 3 and 5 days. At our institution, the average stay after TJA is 3.2 days.
One factor thought to be decreasing the length of hospital stay after TJA is the use of less invasive surgical approaches. Foremost among these is the direct anterior approach for THA. Following the Smith-Petersen interval, this approach is done with the patient in a supine position; its use results in less damage to surrounding muscle.13 It also allows for more rapid mobilization of patients after surgery.
We have begun to use the direct anterior approach more extensively for THA at our institution. We continue to evaluate our experience but expect to find less pain and earlier discharge than with the traditional approaches. Early mobilization has become our mantra for decreasing postsurgery morbidity and complications.
Multimodal Approach to Pain Management
Another reason patients can be discharged earlier is better management of pain after TJA. Several centers rely on a multimodal approach for pain management with the goal of reducing consumption of opiates.
The multimodal approach includes preoperative, intraoperative, and postoperative strategies to control pain. Anti-inflammatories and neuromodulators are given preoperatively, possibly with oral narcotics, to prevent pain preemptively.14 Many TKA surgeons have begun using medicine “cocktails” injected into periarticular tissue intraoperatively. The cocktails often contain local anesthetics and ketorolac, possibly with corticosteroids. Many of the protocols have improved pain control and decreased the use of narcotics after surgery.15
Another new pain management technique is the use of a continuously delivered local anesthetic through a disposable “pain pump.” A catheter is inserted into the intra-articular space after TJA, and medication is delivered at a continuous rate for the first 48 to 72 hours after surgery.
Goyal and associates16 recently presented their findings from a prospective, randomized, double-blind, placebo-controlled study. There was a significant decrease in narcotic consumption in patients who received a pain pump after TKA, and patients' pain scores improved with use of the pump.
Decreased Transfusion of Blood Products
Another important improvement in perioperative management after TJA involves decreased transfusion of blood products. One explanation is the widespread use of regional anesthesia, which has been shown to decrease blood loss and, subsequently, blood transfusion.17
Blood conservation strategies have been implemented to further reduce the need for transfusion. The administration of tranexamic acid (TA) and other agents has become more popular. TA, an antifibrinolytic agent, works by stabilizing clot formation and decreasing blood loss; it can be administered topically or parentally.
The effectiveness of TA in reducing blood loss and the need for transfusion after TKA and THA has been demonstrated in many level 1 studies, which did not find an increase in the incidence of complications, including VTE, associated with the use of TA.18,19 In our practice, TA is given intravenously just before inflation of the tourniquet in TKA and immediately before incision in THA.
HIGHLY CROSS-LINKED POLYETHYLENE
That the bearing surface is one of the most important factors influencing the longevity and functionality of joint replacement has been well established. The use of HCLPE is not a new development; its use in THA has been widespread for almost 10 years. Detailed studies with midterm follow-up, at least in hip replacement, continue to be published. These studies document extremely low wear rates, some cases showing essentially no wear after nearly 5 years of implantation.20,21
A recently published meta-analysis of HCLPE in hips found decreased wear rates compared with those of traditional polyethylene.22 The authors could not demonstrate a difference in the need for revision but speculated that this was only because the follow-up period in the studies they reviewed was too short. Long-term follow-up is expected to demonstrate a lower incidence of revision with the use of HCLPE in THA.
Game-Changer in Hip Replacement
The success of HLCPE truly has been a game-changer in hip replacement. In the face of ongoing problems with other bearing surfaces, HCLPE has been a safe haven for surgeons wanting security and peace of mind for their patients. The promise of a decreased need for revision has given joint surgeons confidence in offering THA to increasingly younger patients who experience degenerative joint disease. There may soon come a time when age is not a factor in evaluating the need for total hip replacement.
This same widespread confidence in the use of HCLPE in THA has been lacking in TKA. Although several in vitro studies have demonstrated improved wear characteristics, detailed clinical follow-up replicating this success is lacking.23,24 However, the paucity of literature confirming the superiority of HCLPE in TKA has not dampened enthusiasm for its use. The necessary clinical research is ongoing.
Like most orthopedic practices, we use HCLPE for TKA. We anticipate that forthcoming evidence will confirm that cross-linking is beneficial for decreasing wear and, ultimately, survivorship of the implants.
CONCLUSION
The practice of joint replacement is not without challenges. Overall, however, arthroplasty continues to improve the lives of hundreds of thousands of patients and the future is bright.
References:
REFERENCES
1. Healthcare Cost and Utilization Project (HCUP). Nationwide Inpatient Sample (NIS). Agency for Healthcare Research and Quality; 1999-2008. http://www.hcup-us.ahrq.gov/reports/factsandfigures/2008/exhibit3_1.jsp. Accessed May 7, 2012.
2. Losina E, Thornhill TS, Rome BN, et al. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg. 2012;94A:201-207.
3. Weinstein AM, Rome BN, Reichmann WM, et al. How many Americans are currently living with total knee replacement? Presented at: American Academy of Orthopaedic Surgeons Annual Meeting; February 7-11, 2012; San Francisco.
4. Falck-Ytter Y, Francis CW, Johanson NA, et al; American College of Chest Physicians. Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 suppl):e278S-e325S.
5. Lieberman JR. The new AAOS clinical practice guidelines on venous thromboembolic prophylaxis: how to adapt them to your practice. J Am Acad Orthop Surg. 2011;19:717-721.
6. Bozic KJ, Vail TP, Pekow PS, et al. Does aspirin have a role in venous thromboembolism prophylaxis in total knee arthroplasty patients? J Arthroplasty. 2010;25:1053-1060.
7. Khatod M, Inacio MC, Bini SA, Paxton EW. Prophylaxis against pulmonary embolism in patients undergoing total hip arthroplasty. J Bone Joint Surg. 2011;93A:1767-1772.
8. Skinner J, Gie G, Kay P. Metal on metal hip replacement and hip resurfacing arthroplasty: what does the MHRA medical device alert mean? British Hip Society newsletter. July 2010. http://www.britishhipsociety.com/docs/Newsletter%20July%202010.pdf. Accessed May 7, 2012.
9. U.S. Food and Drug Administration. Metal-on-metal hip implants. http://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/MetalonMetalHipImplants/default.htm. Accessed March 11, 2012.
10. Langton DJ, Jameson SS, Joyce TJ, et al. Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg. 2011;93B:1011-1016.
11. Hart AJ, Ilo K, Underwood R, et al. The relationship between the angle of version and rate of wear of retrieved metal-on-metal resurfacings: a prospective, CT-based study. J Bone Joint Surg. 2011;93B:315-320.
12. Tiberi JV, Billi F, Kertzner M, et al. Outcomes and pathomechanics of adverse local tissue reactions (ALTR) in metal-metal bearings. Presented at: American Academy of Orthopaedic Surgeons Annual Meeting; February 15-19, 2011; San Diego.
13. Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006;453:293-298.
14. Post ZD, Restrepo C, Kahl LK, et al. A prospective evaluation of 2 different pain management protocols for total hip arthroplasty. J Arthroplasty 2010;25:410-415.
15. Mullaji A, Kanna R, Shetty GM, et al. Efficacy of periarticular injection of bupivacaine, fentanyl, and methylprednisolone in total knee arthroplasty: a prospective, randomized trial. J Arthroplasty. 2010;25:851-857.
16. Goyal N, McKenzie J, Miller A, et al. Efficacy of postoperative intraarticular analgesia following total knee arthroplasty: a randomized, double-blinded, placebo-controlled, prospective study. Presented at: American Academy of Orthopaedic Surgeons Annual Meeting; February 7-11, 2012; San Francisco.
17. Maurer SG, Chen AL, Hiebert R, et al. Comparison of outcomes of using spinal versus general anesthesia in total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2007;36:E101-E106.
18. Alshryda S, Sarda P, Sukeik M, et al. Tranexamic acid in total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg. 2011;93B:1577-1585.
19. Sukeik M, Alshryda S, Haddad FS, Mason JM. Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg. 2011;93B:39-46.
20. Ranawat AS, Tsailis P, Meftah M, et al. Minimum 5-year wear analysis of first-generation highly cross-linked polyethylene in patients 65 years and younger.J Arthroplasty.2012;27:354-357.
21. Bragdon CR, Kwon YM, Geller JA, et al. Minimum 6-year followup of highly cross-linked polyethylene in THA. Clin Orthop Relat Res. 2007;465:122-127.
22. Kuzyk PR, Saccone M, Sprague S, et al. Cross-linked versus conventional polyethylene for total hip replacement: a meta-analysis of randomised controlled trials. J Bone Joint Surg. 2011;93B:593-600.
23. Muratoglu OK, Bragdon CR, Jasty M, et al. Knee-simulator testing of conventional and cross-linked polyethylene tibial inserts. J Arthroplasty. 2004;19:887-897.
24. Lachiewicz PF, Geyer MR. The use of highly cross-linked polyethylene in total knee arthroplasty. J Am Acad Orthop Surg. 2011;19:143-151.




